Table of Contents
Calcium is essential for many biological or physiological processes in the body.
For some reason, there could be a build-up of calcium in body tissues. The breasts are not exempted from this phenomenon. When calcium gets deposited anywhere within the breast tissues, we call it Calcification.
Calcium deposits in the breast are observed in mammograms to be small specks of calcium salts occurring either in clusters or in isolation, anywhere within the breast. It’s usually a sign of noncancerous changes in the breast tissue.
Rarely, do they turn out to be markers of some malignant (Cancerous) processes that raise a lot of concerns that should be addressed as soon as they are detected.
The early detection of these cancerous growths, as published by in a diagnostic manual of breast calcification, Cambridge University Press, is essential to prevent the further spread of tumors and successful treatment outcomes.
Causes of calcium deposits in breast tissues.
- Dead fat cells. Medically, we call it necrosis which refers to the death of some or all cells within a tissue. It could result from physical trauma or a surgical process but is usually benign. Some forms of calcifications resulting from fat necrosis are hard to distinguish from malignant growths.
- Fibroadenomas. As part of what could appear in an abnormal mammogram, these noncancerous growths could at times get calcified.
- Infections like filariasis are known to result in breast calcium deposits which result in calcified worms within the breast tissues according to the Journal of European Radiology.1
- Breast cysts: When calcium gets deposited on very tiny breast cysts, they may appear as clusters of tiny specks suggestive of malignancy but benign.
- The build-up of calcium in the blood vessels of the breast. In research conducted in the Netherlands, the DOM project, as contained in the National Library of Medicine, has associated this with arterial sclerosis.2
- Inflammation. Otherwise called Mastitis is a process that may lead to calcium deposits in breast tissues. This could come on the heels of a trauma, biopsy, and infection as inflammation is a natural body reaction to them.
- Aging process. This explains why these deposits are very common in women above 50 years. The older you get, the higher your chances of having it.
- Trauma. Breast trauma resulting from accidents and even surgical incisions could trigger these deposits.
- Previous cancer treatments. The process of treating breast cancers like surgery and radiotherapy is known to result in tissue trauma or cell death that gets calcified.
- Hereditary factors. It turns out people could be genetically predisposed to this.
- Breast Implants. Apart from scar tissue contractures, calcium deposits may build up around the implant which results in pain. Sometimes the deposits may have to be surgically removed.
- Chronic renal failure. This is rare but has been reported by the British Institute of Radiology (BIR)to trigger calcium deposits in the breast tissues.3
Diagnosis of Calcium deposits in the breast.
Calcium deposits are typically not things you can feel by touch and they are usually symptomless. They are discovered and investigated by the following medical procedures.
Diagnostic mammograms.
This is the first-line approach in their detection. It often comes following the detection of abnormalities in a screening mammogram.
Ductography.
This is performed in patients presenting with symptoms like discharges from the nipples. Ductography involves the injection of dyes for clearer views of the breast ducts. Research published by the American Journal of Roentgenology emphasizes its usefulness as a diagnostic tool.4
Biopsy.
It involves the removal of breast tissues with calcium deposits for investigations. This is achieved in one of two ways.
Stereotactic core needle biopsy.
Done under local anesthesia, meaning only the affected part will be numbed for the procedure to be carried out while you are conscious. A hollow but thin needle is used to get a tiny breast tissue containing a calcium deposit.
This is then used for further investigation and classification. Since the calcium deposits cannot be felt by touch, the process has to be guided by a computerized imaging device like an ultrasound machine.
Surgical biopsy.
It involves using either local or general anesthesia in a theater or doctor’s office. The position of the calcium deposit is first identified and marked before proceeding with the excision of small breast tissue for investigation.
This is employed under certain conditions:
- Failure of core needle biopsy to extract relevant breast tissue.
- Test results following needle biopsy are unsatisfactory.
- Test results after needle biopsy show the existence of abnormal cells.
Magnetic resonance imaging (MRI) and Ultrasound:
Though calcium deposits usually don’t show in any of these types of equipment, they could be done in a few cases to detect tissue changes that may be cancerous.
Kindly keep in touch by signing up for my Newsletter:
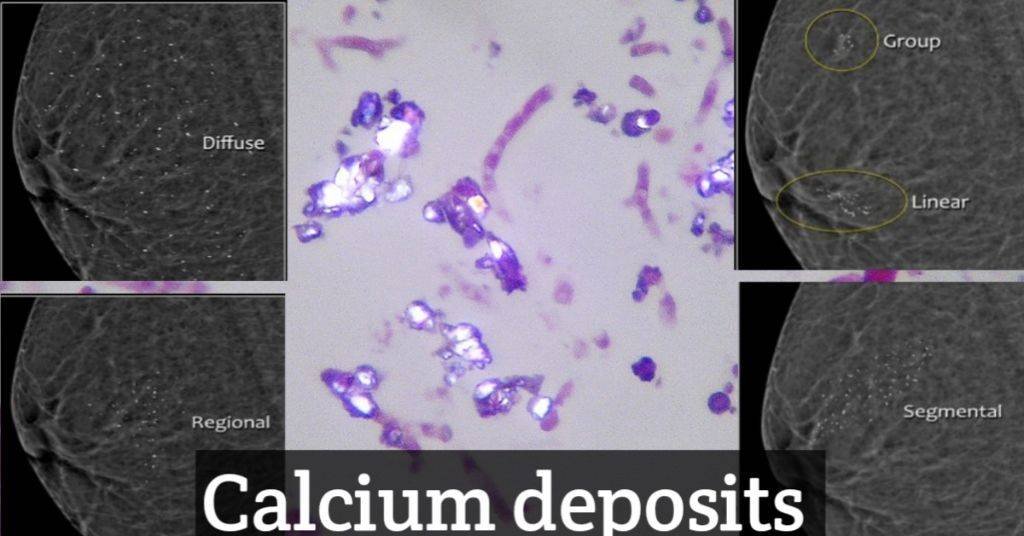
Types of calcium deposits.
There are two types.
Macro calcium deposits.
These are comparatively larger noncancerous(benign) deposits of calcium shown in mammograms as randomly dispersed dots in the breast tissue. There is a 50% chance you have them if you are above 50 years old and a 10% chance below 50.
Micro calcium deposits.
They are comparatively smaller calcium deposits with the semblance of white specks on mammograms. They too are usually not cancerous but become suspicious when they show certain characteristics like clustering, certain patterns, or morphology (that is, certain shapes).
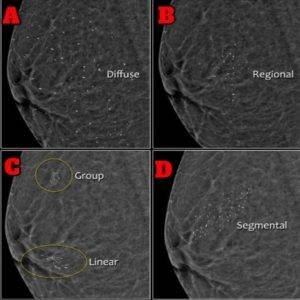
Note that some women present with both micro and macro-calcium deposits in their breasts.
Classification of calcium deposits.
With the discovery and examination of your breasts’ calcium deposits, they are placed in one of three classifications.
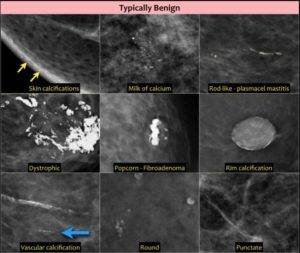
Benign.
These have been confirmed as non-cancerous, requiring no further follow-up or tests. Of this, you’ll have to revert to your regular screening mammograms. Your calcium breast deposits are taken to be benign if they are observed to have the following morphology(shape) or location:
- Round and punctate (appear like dots),
- Lucent-centered,
- Dystrophic deposits,
- Eggshell or Rim,
- Large Rod-like,
- Coarse or popcorn-like,
- Plasma cell mastitis,
- Skin calcium deposits,
- Milk of Calcium,
- Vascular calcium deposits,
- Suture calcium deposits, etc
Probably benign calcifications or calcium deposits.
These are found to need monitoring twice a year for at least one whole year though there is a less than 2% chance they’ll turn out cancerous. Calcium deposits that fall in this class are those with a morphology seen to be:
- Amorphous (without defined shape), otherwise called Amorphous calcification.
- Coarse heterogeneous.
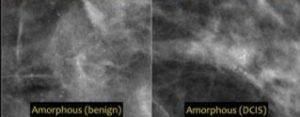

Benign calcium deposits are generally seen to be larger than 0.5mm, with well-defined morphology and not clustered.
Suspicious deposits.
A biopsy is called for in this class of deposits because they are likely cancerous. Calcium deposits fall into this class when they are observed to have the following shape:
- Fine Pleomorphic.
- Fine linear.
- Fine linear branching.

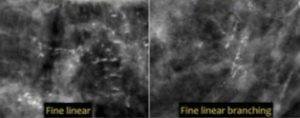
Cancerous calcium deposits are generally seen to be smaller than 0.5mm, have varying morphology, and are found to be clustered.
Calcium deposits and Breast cancer.
Calcium deposits are markers of noncancerous underlying physiological processes in the breasts. They don’t turn into cancer Click To Tweet and are usually symptomless unless other things are happening concurrently or may have happened in the same area like existing implants.
Rarely, they may signify malignant (Cancerous) processes in the breast. At times they may be the only sign of cancerous growth in many women who have had to undergo more tests following observations made on mammograms.
These include those who may have been diagnosed with conditions like ductal carcinoma in situ (early-stage cancer). This underscores the importance of mammography as early discovery and early treatment save lives.
Removal of calcium deposits in the breast.
Once they are told of the detection of calcium build-up in their breasts some women freak out. They are like……Oh my God, something is building up in my breasts, how do I remove it?
Why do you want to bother with something harmless when any attempt to get rid of it will result in surgical trauma and inflammation that also causes it?
In truth, you don’t have to bother with it and this applies to the majority of cases. Rarely will they be of any medical or health concern. You wouldn’t even have ever known they were there if not for mammography.
Let me know if this article was satisfactorily helpful. However, if it didn’t serve your interests, also get me informed about areas I may have overlooked that you cared about.
References.
- Bastarrika, G., Pina, L., Vivas, I. et al. Calcified filariasis of the breast: report of four cases. Eur Radiol 11, 1195–1197 (2001). https://doi.org/10.1007/s003300000711 ↩︎
- de Waard F, Collette HJ, Rombach JJ, Baanders-van Halewijn EA, Honing C. The DOM project for the early detection of breast cancer, Utrecht, The Netherlands. J Chronic Dis. 1984;37(1):1-44. doi: 10.1016/0021-9681(84)90123-1. PMID: 6690457. ↩︎
- S. E. Evans and G. H. Whitehouse. (2014). Extensive calcification in the breast in chronic renal failure. British Journal of Radiology. Vol. 64, No. 764. https://doi.org/10.1259/0007-1285-64-764-757 ↩︎
- G Cardenosa, C Doudna, and G W Eklund. (1994). Ductography of the breast: technique and findings. American Journal of Roentgenology.Volume 162, Issue 5. https://doi.org/10.2214/ajr.162.5.816598. ↩︎