Table of Contents
Arthritis typically has no cure but is treated to manage the symptoms, reduce disease progression, and maintain mobility, and quality of life. The choice of treatment for arthritis in the knees is guided by a couple of factors that include the type of arthritis, stage of the disease, comorbidities, age, and needs.
The joint at your knees is formed by three bones namely the femur, tibia, and patella otherwise called the knee cap. These bones are more prone to three main types of arthritis. These are:
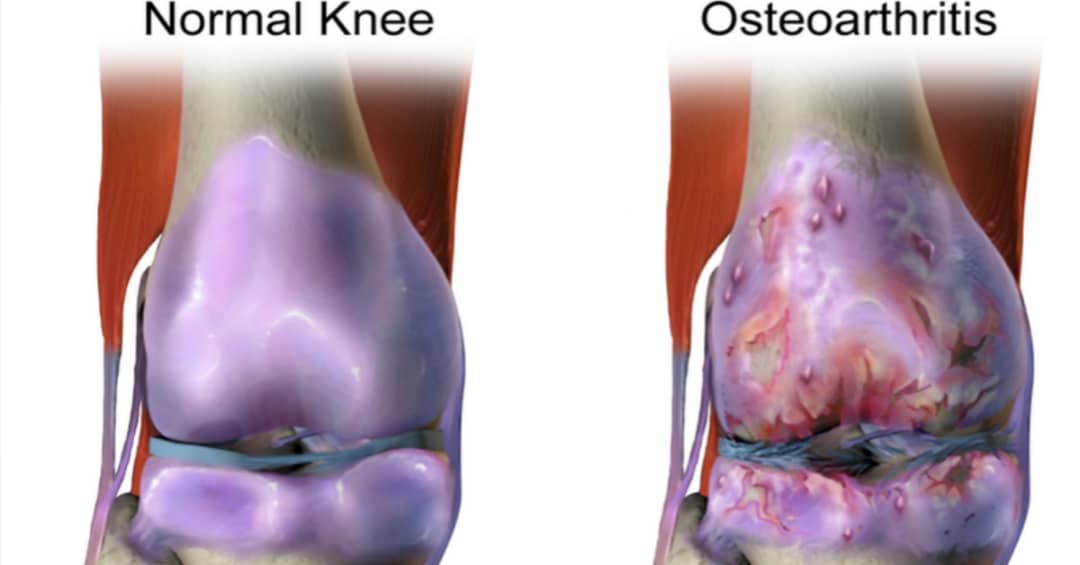
- Osteoarthritis: This is a degenerative type of arthritis that eventually leads to the breakdown of the articular cartilage that lines the ends of the bones that make up the knee joint. The risks are higher with age, especially for those above 50 years.
- Rheumatoid arthritis: It is triggered by an autoimmune reaction whereby your body’s antibodies attack the lining of your knee joint as it sees them as foreign material. The synovial membrane that ensures the lubrication of your joint becomes inflamed as a result. The affectation is not age-specific. It could occur at any age.
- Post-traumatic arthritis: As the name suggests, this type of knee arthritis happens as a result of a previous injury to any of the structures within or near the knee joint that impacts its normal function. Injuries that affect the bones, ligaments, articular cartilage, or tendons could trigger this type of arthritis.
Several factors leave you prone to this arthritis. Most of these have been highlighted in the arthritis of the fingers so we won’t list them here since the same factors still apply to arthritis in the knees.
The treatment of arthritis in the knees is mostly about managing the symptoms. We’ll progress with discussing some of these symptoms that make arthritis a terrible disease.
Symptoms of knee arthritis.
Here are most of the common symptoms you’ll expect when you have arthritis in the knees.
Pain: This is the worst of the symptoms and could be worse in the mornings or after moderate to high-intensity activities.
Crepitus: This is the abnormal grinding, cracking, grating, or clicking sounds the joint makes during movement. It is often audible but I usually place my palm firmly on the knees when checking for this during a physical examination of a patient. Crepitus may not be accompanied by pain.
Joint swelling: This is normally due to fluid collection around the joint.
Joint stiffness: It may be worse in the morning or after a period of inactivity. Usually gets better with activities or exercises.
Warmth around the affected knee: It’s one of the components of inflammation.
Redness: This is part of an inflammatory process but if you are dark-complexioned it may not be so obvious to you.
Joint deformity: It takes time to get to this stage and may result in deformities like genu varum(bowleg) among others, on a once normal knee.
Reduced active and passive range of motion: Passive range is the range the knee could be bent or stretched by an applied external effort whereas active range is the one you could achieve when you move the joint by your muscles. Both of these ranges get increasingly affected as the disease progresses.
Knee pain from arthritis.
Knee pain from arthritis is a major reason for all the worries, hospital visits, and treatment expenses that go with the disease. You can bet people will be less bothered if the disease is pain-free.
The pain may not be the very first symptom you will feel. It may come gradually in an on-and-off pattern but builds in intensity with time as well as becomes sustained or lasts longer. Initially, you may only feel pain after certain activities that put stress on the knees but as the disease progresses you start feeling it even at rest.
Activities that may bring on the pain include:
- Running,
- Jogging,
- Squatting,
- Bending,
- Stair climbing,
- Weight-bearing exercises or workouts,
- Prolonged rest or inactivity.
The above-listed activities could lead to flare-ups but their impact will also depend on the actual type of arthritis you have.
Some activities may bring you some relief such as:
- Gently massage the sides of the painful knee. Though better with a topical analgesic. This may not make a difference in more advanced cases.
- Gentle non-weight-bearing knee exercises like swinging your legs in mid-air. You could do this while seated on something high enough for your feet to hang freely in the air,
- Rest from activity when it hurts.
- Application of ice during a flare-up,
- Application of some warmth around the joint with something like a hot water bottle when the pain isn’t due to an inflammatory process.
- Shedding some weight and keeping to your right body mass index(BMI).
Kindly keep in touch by signing up for our newsletter:
Knee arthritis treatment without surgery.
Surgery is the last option in the treatment of osteoarthritis and is only considered when all other options fail or have become ineffective in managing the symptoms. Non-surgical measures include:
- Medications, vitamins, and supplements,
- Physical or occupational therapy interventions,
- Lifestyle modifications, diets, and weight loss,
- Low-level laser therapy, and
- Alternative therapies like acupuncture.
Medications.
Medications are among the first line of interventions. This is also in line with standard recommendations for the treatment of arthritis associated with autoimmune problems like rheumatoid and psoriatic arthritis.
The medicines found to be effective in giving you relief include:
- Acetaminophen,
- Non-steroidal anti-inflammatory drugs,
- Corticosteroids,
- Phosphodiesterase-4 inhibitors(PDE4),
- Disease-modifying anti-rheumatic drugs and biological agents.
The last two items in the list are normally employed when dealing with arthritis of autoimmune origin like rheumatoid.
Useful vitamins and supplements that help with symptoms of knee osteoarthritis are vitamins A, E, and K plus omega-3 fatty acids. Supplements containing these and other substances like glucosamine chondroitin sulfate, Methylsulfonylmethane (MSM), S-adenosyl-L-methionine, and Hyaluronic acid can also help manage your symptoms.
As someone who not only treats arthritic patients but also lives with osteoarthritis of the knees, I can tell from experience these work but not in the absence of other measures like weight loss and some kind of diet restrictions.
Note that whatever relief you can get from these will depend on the stage of your osteoarthritis. There may come a time when none of these will make any significant difference in your symptoms as the disease progresses.
Exercises for arthritis in the knee.
Exercises are a key part of a physical therapist’s intervention. While you still have healthy knee joints you could do a lot more types of workouts but not when you develop knee arthritis. Engaging in some kind of workout could lead to flare-ups which is something you should avoid.
Exercises that may be recommended include:
Muscle strengthening exercises,
- Cycling,
- Stretching,
- Walking,
- Hydrotherapy(an aspect of physical therapy where you do workouts in a pool),
- Aerobics, and
- Pain relieving measures in some cases.
Usually, they should be low-intensity workouts but your physical therapist doctor is in the best position to make the right recommendations after duly examining you. Not every exercise is right for everyone even if you all have a similar type of knee arthritis.
In the video below are useful exercises you could do on your own at home. Your physical therapist may teach you their modifications.
Weight loss.
If you have knee arthritis and you are overweight or obese, the importance of weight loss cannot be overemphasized. The knees are weight-bearing joints but with a disease like arthritis the amount of weight they can handle without symptoms drops and keeps reducing as the disease progresses.
If you struggle with weight management, your doctor could help you with an effective medical weight-loss plan.
Weight loss alone isn’t enough for the management of arthritis, a publication in the National Center for Biotechnology information shows it has to be combined with exercises as mentioned earlier for a better outcome.
Orthotic devices.
These are braces and splints used to provide support, stability, and redistribution of weight in an arthritic knee.
A brace designed to provide support and stability will usually be firm with no hinge at all or come with double hinges. One that’s designed to redistribute your weight to ease symptoms that’s on one side of the knee will usually have just one hinge.
The latter are called unloaders and what I described above is an easy way of differentiating them from other braces. Unloaders help to transfer more of your weight to the side or compartment of your knee that’s not hurting. Osteotomy does the same thing.
The focus in the use of unloaders is often the redistribution of weight between the lateral and medial compartments. However, three compartments make up the knee joint namely:
- Medial femorotibial compartment,
- Lateral femorotibial compartment, and
- Patellofemoral compartment.
Your physical therapy doctor or physician should be able to recommend the right device for you after a physical examination.

under creative c.
Low-level laser therapies.
Research contained in the National Library of Medicine has found this very useful in the treatment of osteoarthritis of the knee as a result of its analgesic and microcirculatory effects. The research result showed very significant improvement in the following areas:
- Knee joint flexion,
- Sensitivity to pressure, and
- Reduced joint pain.
In a clinical trial, a total of 8 points around the knee were used for a 20-minute irradiation with low-level laser therapy with a wavelength of 850nm. 3 points each were chosen at the medial and lateral aspects of the knee while the remaining 2 were placed at the popliteal fossa at the medial side of the biceps femoris and semitendinosus muscle tendons.
Another published work in the National Library of Medicine showed low-level laser therapy reduces disability and pain in osteoarthritis of the knee at the following treatment parameters:
- At 4-8 Joules with a wavelength of 785-860 nm,
- At 1-3 Joules with a wavelength of 904 nm.
Alternatives therapies.
Other non-surgical and perhaps non-medical approaches to the treatment of arthritis in the knee include:
- Acupuncture,
- Homeopathy, and
- Yoga.
Acupuncture and yoga, where they fail to help, are not expected to have any side effects when done properly. Homeopathy uses non-conventional medications to treat arthritis and there are mixed reports on its efficacy.
A Journal article in the British Society for Rheumatology suggests it’s the homeopathy consultation that yields clinically relevant positive outcomes rather than homeopathic drugs.
Surgical intervention.
Surgery is usually the last option in any case of knee arthritis and literally in most other medical conditions. There is a significant risk to it but the benefits usually outweigh the risks otherwise it may not get a green light, especially in cases with 50-50 chances of success or failure.
With advances in medical practice, there is a paradigm shift from more invasive to less invasive surgical procedures. This has significantly reduced the risks associated with a lot of surgical processes.
Reasons for surgery in the treatment of arthritis in knees.
With the incurable nature of arthritis, every intervention given is meant to bring you relief and where possible, halt the progression of the disease. Surgery is only considered when the interventions mentioned earlier fail to achieve results or have stopped working.
The aim of surgical intervention as contained in an article in the European Orthopaedic and Traumatology Journal, is the restoration of a durable pain-free, and functional knee joint.
Don’t get things twisted about pain. There will be a period of post-surgical pain and discomfort but it may not last beyond a couple of weeks or a few months. How long it lasts depends on how invasive your surgery is.
Secondly, depending on the type of surgery, it’s not unusual to feel little discomfort even if intermittently and the knee will certainly never feel exactly as good as the normal one. Be that as it may, you’ll be happy you had the surgery and should be able to resume normal life afterward.
Types of surgery.
Factors used in determining the most appropriate surgery for you, as contained in the National Institute of Health, include:
- Stage of the disease,
- The location or compartment,
- Presence of comorbidity.
Surgical interventions range from arthroscopy to total knee joint replacement.
Tibial or femoral osteotomy.
Osteotomy of the tibia or femur achieves the aim of the use of an unloader brace but in a surgical way. It applies if your arthritis is only in or worse in one compartment of your knee. These are usually the medial or lateral ones. The operation may also help halt or slow down the progress of your arthritis.
Being active, under 60 years, with pain only on one side of your knee, and having the right range of body weight or body mass index(BMI), are other Important factors that make this procedure right for you.
In an osteotomy, the surgeon cuts into your tibial or femur to remove or add a piece of bone graft or an artificial bone object that’ll help shift some of your body weight away from the damaged compartment.
Injury to the neurovascular bundle(the nerves and blood vessels that run through the back of the knees) could occur and is the worst complication that may result as contained in the Journal of Sports Medicine and Arthroscopy Review. However, this is uncommon.
Knee arthroscopy.
It’s a minimally invasive surgery and involves the use of an instrument called an arthroscope which is a type of video camera used in viewing the inside of your knee joint.
The arthroscope and other surgical instruments are passed into the joint through a small incision made by the surgeon. With this tool, the extent of damage to the knee could be seen. During this procedure, knee debridement and lavage could be done which may bring you some relief.
Not everyone believes knee arthroscopy should be viewed as a type of treatment for arthritis.
Debridement.
This process involves the removal of an inflamed synovial membrane, loose osteophytes or cartilage, and smoothening of surfaces that have been roughened by arthritis.
These things are usually responsible for much of the symptoms you may be having and patients often feel better afterward. Nonetheless, it doesn’t halt the progression of knee arthritis.
Lavage.
This is simply the use of a saline(salt) solution to flush the knee joint thereby removing loose particles that may be contributing to arthritic inflammation.
Cartilage repair surgery.
This process can only be used in the event of focal(small area) damage to the articular cartilage(Karolin Ronn et al) as contained in a review article titled Current Surgical Treatment of Knee Osteoarthritis. Since cartilage almost has little or no ability to heal, this surgery aims to achieve just that. It could help slow an arthritis process, preventing it from entering worse stages of the disease.
Younger people stand to benefit from this than older ones who may already be battling with a significant level of knee arthritis. Current techniques employed in cartilage repairs are detailed in the National Library of Medicine database. Some of these are:
- Microfracture(MF),
- Drilling,
- Autologous chondrocyte implantation(ACI),
- Osteochondral allograft(OCA), and
- Osteochondral autograft transplant(OAT).
The size of the lesion could influence which technique could serve you best as shown in the table below:
| Size of cartilage damage or lesion. | Preferred repair technique. |
|---|---|
| Less than 2cm. | MF or OAT. |
| 2-4cm. | OAT or ACI. |
| Greater than 4cm. | ACI or OCA. |
Partial knee replacement surgery or unicompartmental arthroplasty.
This is applied where only one compartment in the knee joint is damaged by arthritis which is most likely the medial or lateral compartment. It involves the replacement of the damaged compartment with an artificial construct or prosthesis.
You may not be considered for this procedure if:
- Your arthritis is due to an autoimmune disease.
- You have any of genu valgum(K-leg) or genu varum(bowleg) knee deformity.
- You have damaged knee joint ligaments.
- The affected knee joint has a high level of stiffness.
Total knee replacement surgery or arthroplasty.
It is the most pain-relieving surgical intervention available and involves the replacement of the entire arthritic knee joint with an artificial one as has been described on MedlinePlus. The artificial joint is normally chiefly made from either metal or plastic. This operation is considered for people with moderately severe to severe arthritis in the knee joint on whom none of the nonsurgical approaches can help anymore.
As effective as it may be, the artificial joint is not as durable or strong as the natural joint. For this reason, it may not be the best for highly active people or those who may get into high-impact activities or sports. You’ll normally be given these as precautions that will ensure the prosthesis lasts.
Final words.
Arthritis is a distressing and debilitating medical condition and the knees are one of the worst places it could happen to you. Unfortunately, it’s one of the most common joints it occurs especially osteoarthritis.
It’s an incurable yet progressive disease so you need to do everything you can to slow it down with the help and guidance of your healthcare provider. This article was only meant to get you informed about the disease and if it has been helpful please don’t hesitate to share it.