Table of Contents
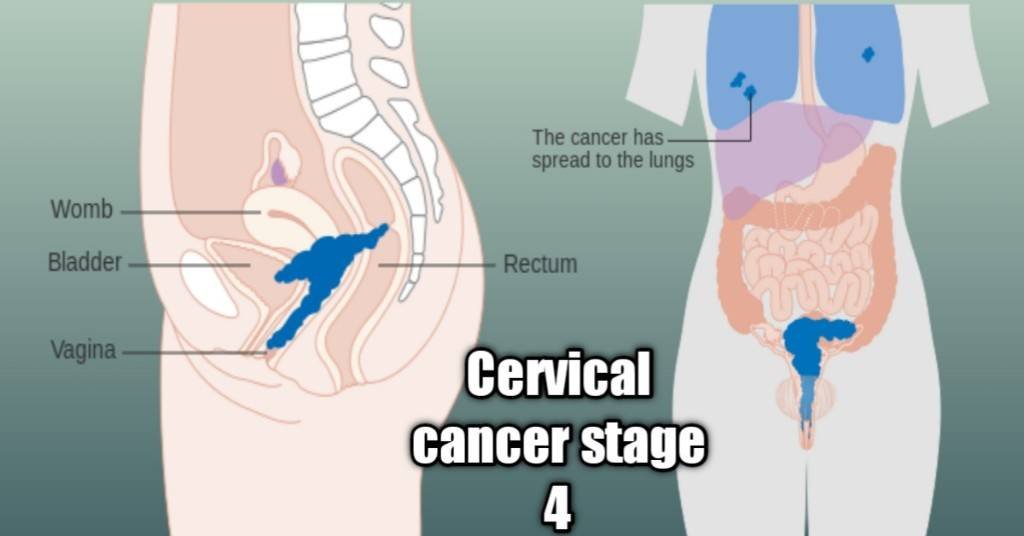
Cervical cancer stage 4 is cancer that has spread beyond the cervix to either neighboring tissues and organs (locally advanced) or has metastasized to more distant parts of the body like the lungs and bones.
It could take as much as 10 to 20 years to get to this point if you have strong immunity or as little as 5 years with weakened immunity.
It is usually discovered with an abnormal pelvic examination accompanied by well-known symptoms that are characteristic of cervical cancer. You could more likely end up with this stage of cancer if you aren’t going for regular screening tests but only show up at a point when you become sick with the symptoms.
Early detection is key to the survivability of cervical cancer and the avoidance of the horrific consequences of this cancer stage. However, cancers detected early at times progress to this stage even with treatment.
There are two sub-stages of cervical cancer stage 4 and they are 4A and 4B.
Sub-stage 4A
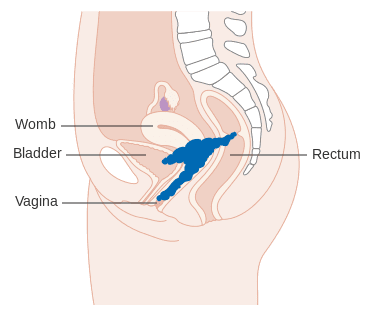
This stage describes when cancer has spread beyond the pelvis to nearby tissues and organs such as the bladder, rectum, and lymph nodes but hasn’t left the pelvic area to more distant body parts. (source)
It falls in the category of locally advanced cervical cancers which describes all the stages from 1b2 to this stage, 4A.
I take stage 4A as the last stage where treatment can reasonably be administered with the aim of a cure (even if it wasn’t achieved) rather than as palliative.
Sub-stage 4B
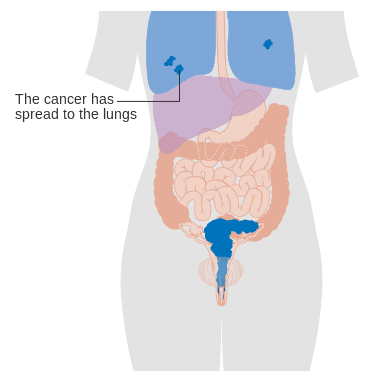
This is the last stage describable. At this point, cervical cancer has metastasized from the pelvic region to distant parts of the body or organs such as the lungs, bones, and liver. The prognosis at this stage is the worst that can be expected as it’s complicated to treat.
The symptoms can be severe, and treatment objectives often boil down to palliative care. No matter how far it goes or what organ gets affected, it remains cervical cancer descriptively. For instance, that it spreads to the lungs and starts growing there doesn’t translate to lung cancer but rather cervical cancer.
That’s because cancers are named based on their origin rather than where they were able to spread in the course of metastases.
Symptoms and what to expect.
Early stages of the disease are usually asymptomatic (not showing any symptoms) but it is common to discover stage 4 cervical cancer following an abnormal pelvic examination with some or all of the following symptoms as Published by the National Institute of Health (NIH):1
- Foul-smelling vaginal discharge that could be watery, pinky, brownish, or bloody.
- Unusual vaginal bleeding between menses and after coitus (intercourse).
- Pelvic pains, which could also happen after intercourse.
- Nausea.
- Loss of appetite.
- Fever.
- Fistula.
- Leg swelling.
- Fatigue or tiredness.
- Diarrhea.
- Shallow breathing is characterized by a reduced tidal volume (that is the volume of air leaving or entering the lungs).
- Constipation.
- Muscle atrophy (wasting) and weakness.
Some of these symptoms may also result from treatments being administered.
Kindly stay in touch by signing up for my newsletter:
Treatment of cervical cancer stage 4.
The particular treatment you receive is determined by the location of cancer in your body, the type of cells involved, and your state of health concerning your tolerance of the procedure.
There are 4 options in your treatment which are:
1. Radiation therapy,
2. Chemotherapy,
3. Vascular endothelial growth factor (VEGF) targeted therapy according to the Journal of the Polish Society of Obs&Gyne, Ginekologia.2
4. Surgery like a pelvic exenteration, as published in the American Journal of Surgery.3
Treatment choice is often a combination of any of the above 4 options like in Chemoradiotherapy.
This could involve the administration of about 25 doses of external Radiotherapy once daily for about 5 weeks (5 per week) and a course of chemotherapy weekly or once every 2 to 3 weeks according to Cancer Research, UK (CRUK).
At the end of treatment, you could also be given internal radiotherapy otherwise called Brachytherapy. Brachytherapy involves the use of radioactive materials to deliver doses of radiation targeting cancer directly. There are two types:
1. Temporary brachytherapy or High-Dose-Rate Brachytherapy (HDR): A radioactive seed is inserted close to the tumor to deliver high-dose radiation for about 10 to 15 minutes.
2. Permanent brachytherapy or Low-Dose-Rate Brachytherapy(LDR): In this type, the radioactive seed is planted permanently in your body to keep delivering low-dose therapeutic radiation to the tumor. The radioactivity wanes over time.
The American Brachytherapy Society recommends High-Dose-Rate brachytherapy for treating cervical cancer.4
In the European Journal of Surgical Oncology, primary exenteration has been described as a valid option for chemoradiation.5 Secondary exenteration surgeries are recommended for recurrent cancers that remain confined within the pelvis.
Despite the combination of treatment modalities, a good number of patients with stage 4 cervical cancer do have relapses Click To TweetTreatment for sub-stage 4A
With the tumor spreading beyond the cervix to neighboring tissues and organs within the cervix the most likely treatment plan will be chemoradiotherapy. That is a combination of chemotherapy and radiation to achieve a cure.
For recurrent cancer that is still confined within the pelvis, exenteration surgery may be considered but this will not happen until an extensive medical evaluation is done to see the possibilities of carrying out such a very major surgery and your chances of survival.
Exenteration surgeries involve several specialist surgeons which indicates how major it is. There are 3 types of pelvic exenterations which are:
1. Anterior Pelvic exenteration surgery. This refers to the surgical removal of all or part of the vagina along with the cervix, uterus(womb), lymph nodes, fallopian tubes, ovaries, and the organ in front of the vagina which is the bladder with its ureter.
The anus and rectum are spared. To maintain your ability to expel urine from the body a urostomy is created that makes this possible. The process for this is explained in the video below
Your urine is emptied a couple of times a day via a urostomy bag
2. Posterior Pelvic exenteration. In the posterior, all or part of the vagina is taken out along with the cervix, uterus, fallopian tubes, ovaries plus the rectum and anus located at the back of the vagina.
This time the bladder and ureter are spared so you won’t need a urostomy and its bag for urine collection. Great, isn’t it?
However, because of the removal of the anus and rectum, there’ll be a need for another kind of stoma called a colostomy. This is designed to evacuate feces as described in the video below without which there will certainly be a problem.
3. Total pelvic exenteration. I believe you’ve noticed the difference between the anterior and posterior pelvic exenteration surgeries lies in the area that is spared relative to the vagina.
Anterior means front and stands for the removal of structures in front of the vagina (bladder and ureter) whereas posterior means back and means the removal of structures at the back of the vagina (anus and rectum).
A total pelvic exenteration surgery represents the removal of the bladder, rectum, and all other things removed in earlier types like the cervix, uterus, fallopian tubes, ovaries, and all or part of the vagina.
In any of the two previous exenteration surgeries, you may have been spared a urostomy or colostomy. In total exenteration, you’ll have to deal with both. Some facilities may combine the two so you’ll have one stoma for both types of waste products (feces and urine). (source)
Unlike hysterectomy which could be done in a way that preserves fertility, pelvic exenteration has no room for that as it renders patients barren.
What is going through my mind right now as I type this is how mothers are increasingly becoming agents of opposition to the human papillomavirus vaccinations, citing safety concerns as published in a previous article you may want to read. Though it is generally believed these vaccines are quite safe, a recent finding published in the New England Journal of Medicine (NEJM) suggests cancer vaccines should be investigated.6
We first made this known in a retweet on one of our social media handles. You may want to follow us on that channel and scroll down to join our other social media networks for continuous updates.
Mothers who refuse to get their girls duly vaccinated put these girls at risk of losing the same organs without which they would never have become mothers. Which is safer, getting your girl-child vaccinated and placing her at risk of cervical cancer later in life?
Treatment for sub-stage 4B
At this stage, cancer has been found to have spread beyond the organs and tissues in the pelvic area to distant parts of the body like the lungs, liver, bones, etc. The preferable approach to treatment is usually the combination of Radiotherapy and Chemotherapy otherwise called chemoradiotherapy.
This is the terminal stage and the most difficult to treat. The majority of patients that get to this level don’t make it no matter the kind of treatment given and the intensity.
Surgery isn’t considered an option unless it is done for palliative reasons to relieve symptoms such as pelvic sepsis, foul smell, pain, and obstructions. This type of surgery is called pelvic palliative exenteration (PPE) surgery and is published in the European Journal of Surgical Oncology. Some professionals don’t support the idea though.
The aim of treatment at this stage is usually focused on palliative care with the following objectives:
- Relieve the patient’s symptoms as much as possible.
- Maintain quality to any extent possible.
- Keep the patient as active as can be.
- Get the patient to live for as long as possible.
- Ensuring the patient doesn’t suffer neglect.
- Prepare the minds of loved ones for the inevitable.
- Ensure all essential medications and supplies are provided.
- Prevention of rapid deterioration, complications, or management of complications if they occur.
- To educate loved ones on how best to care for a patient with a worsening condition.
The World Health Organization (WHO) has given extensive details on what the ideal palliative care should entail.7
Prognosis or survival rate.
Only about 15% of people with this terminal stage of cervical cancer are known to live for the next 5 years from the date of diagnosis according to Cancer Research, UK. This is a far cry from an over 80% survival rate for people with early-stage cancer as discussed in another article you may want to read.
A lot may not live beyond 1 or 2 years from the time of diagnosis but some surpass that timing. However, I believe what is most important isn’t how long but how well. Less than 3 years with a relatively good quality of life and minimal distress is better than extra years with excruciating pain and suffering.
If you are female, you may also want to find out a thing or two about breast cancer.
References.
- Comprehensive Cervical Cancer Control: A Guide to Essential Practice. 2nd edition. Geneva: World Health Organization; 2014. 7, Palliative care. Available from: https://www.ncbi.nlm.nih.gov/books/NBK269626/ ↩︎
- Magdalena Salomon-Pierzyńska, Beata Rembielak-Stawecka, Bogdan Michalski, Aleksander Perzyński, Violetta Skrzypulec-Plinta. (2014). VEGF – targeted therapy for the treatment of cervical cancer – literature review. Ginekologia Polska. Ginekologia Polska. Vol 85, No 6. #45878. DOI: 10.17772/gp/1754. Available from: https://journals.viamedica.pl/ginekologia_polska/article/view/45878 ↩︎
- Brophy, P. F., Hoffman, J. P., & Eisenberg, B. L. (1994). The role of palliative pelvic exenteration. The American Journal of Surgery, 167(4), 386-390. https://doi.org/10.1016/0002-9610(94)90121-X ↩︎
- Nag, S., Erickson, B., Thomadsen, B., Orton, C., Demanes, J. D., & Petereit, D. (2000). The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix. International Journal of Radiation Oncology*Biology*Physics, 48(1), 201-211. https://doi.org/10.1016/S0360-3016(00)00497-1 ↩︎
- Hidde M. Kroon, N.N. Dudi-Venkata, S. Bedrikovetski, M.L. Thomas, M.E. Kelly, et al. (2019). Palliative pelvic exenteration: A systematic review of patient-centered outcomes. European Journal of Surgical Oncology, 45(10), 1787-1795. https://doi.org/10.1016/j.ejso.2019.06.011 ↩︎
- Weber JS et al. Individualized neoantigen therapy mRNA-4157 (V940) plus pembrolizumab versus pembrolizumab monotherapy in resected melanoma (KEYNOTE-942): A randomized, phase 2b study. Lancet 2024 Jan 18; [e-pub]. (https://doi.org/10.1016/S0140-6736(23)02268-7. opens in new tab) ↩︎
- Comprehensive Cervical Cancer Control: A Guide to Essential Practice. 2nd edition. Geneva: World Health Organization; 2014. 7, Palliative care. Available from: https://www.ncbi.nlm.nih.gov/books/NBK269626/ ↩︎