Table of Contents
The human papillomavirus is a major health concern as it is known to be the most common viral sexually transmitted infection in the US and around the world. It is found in more than 99% of cervical cancers according to the UK’s National Health Service (NHS).
Vaccines don’t cure HPV but are designed for preventive or defensive purposes by keeping your body ready for any eventual encounter with the virus, as contained in the US National Library of Medicine (NLM).1
In this article, we’ll examine the effectiveness and other factors regarding Gardasil for HPV
The development of the Gardasil vaccine.
The first available scientific literature on cervical cancer research dates as far back as 1840 as contained in the National Library of Medicine (NLM) but it wasn’t till the 1970s that a German virologist, Herald Zur Hausen, was able to extract the human papillomavirus from cervical cancer.2
This confirmed earlier suspicions of HPV as the cause of cervical cancer. Unfortunately, the pharmaceutical companies turned down his call for the production of vaccines for the prophylaxis of cancer in 1986 on the grounds it wasn’t profitable (It’s sad to know profit comes first before lives in today’s world).
The first vaccine was developed in Australia at the University of Queensland by two professors, In Frazer and Jian Zhou. This they achieved through the successful synthesis of virus-like proteins (VLP) in 1990 used in making the vaccines. This led to the manufacturing of the Gardasil vaccine which was eventually approved for public use by 2006 after undergoing the due processes of clinical testing and trials.
Ingredients of Gardasil.
The Gardasil vaccine as you may have now realized from the above section isn’t made directly from the HPV virus. In other words, it doesn’t contain the actual HPV virus and is non-infectious. Though current ones are made differently and are highly immunogenic (ability to induce immune responses), they are still noninfectious.
The virus-like particles (VLP) proteins were originally produced from yeast cells by a process called recombinant DNA technology which uses enzymes to split and join DNA sequences of interest from different sources as contained in the National Human Genome Research Institute.
The Ingredients, according to the Food and Drug Administration (FDA), are.
- Virus-like Proteins, (VLP).
- Amorphous aluminum hydroxyphosphate Sulfate (An adjuvant to prolong its efficacy).
- Yeast protein.
- Sodium chloride (common salt).
- L-histidine (an amino-acid, protein).
- Polysorbate 80 (a synthetic nonionic surfactant).
- Sodium borate (a powdery white substance also known as Borax).
- Injection water (the sterile version).
Types of HPV vaccines.
There are 3 types of these vaccines according to the Centers for Disease Control and Prevention: government authority (CDC) :
- Bivalent HPV vaccine(2vHPV). Otherwise called Cervarix.
- Quadrivalent(4vHPV). Known as Gardasil.
- Nanovalent(9vHPV). Commonly called Gardasil 9.
One thing common among these vaccines is that they all offer protection against HPV-16 and HPV-18 which are responsible for cancers.
The Cervarix vaccine’s protection doesn’t go beyond those two and it is termed Bivalent, meaning specificity for two human papillomavirus strains HPV-16 and 18 which are the principal culprits for cervical cancer. Quadrivalent (Gardasil) is specific for 4 types of HPV infections.
Something tells me you’ve already figured out, in your intelligence, that Gardasil 9 deals with an extra 5 types of HPV infections.
Methods of administration.
Our vaccines of interest are designed for intramuscular injections (IM, for short), as covered by the Centers for Disease Control and Prevention (CDC). There are four common sites for IM injections which are:
- Deltoid muscles.
- Ventrogluteal muscle.
- Vastus lateralis (one of the large muscles of your thigh)
- Rectus femoris muscle (also of the thigh).
Among these four possible muscles for intramuscular injection, the best site for an HPV vaccine is the deltoid muscles of your upper arm followed by the vastus lateralis muscle.
HPV vaccines are not recommended to be given intravenously, subcutaneously, or under the skin (intradermally).

Indications and contraindications to vaccinations.
Just as we have it in other vaccinations, the HPV vaccines also have their list of indications and contraindications.
Indications:
It’s indicated for the prevention or prophylaxis of most human papillomavirus-mediated processes that could lead to genital warts or various cancers in both sexes (source) and recommended for administration on:
- Preteens (11 to 12 years). 9-year-olds are also eligible.
- Teens who either didn’t complete their vaccine dosages or never started.
- Adults above 26 years who also didn’t complete their dosages or never had.
Contraindications:
1. The vaccines are not recommended for use in pregnancy. You should plan for your baby shower instead if you are pregnant. There are lots of other medications and indulgences you need to place on hold especially in the first few months of pregnancy for the sake of your baby.
If you are not yet pregnant but planning to, that plan should be on your list of topics for discussion with your doctor while considering vaccination.
2. If you are allergic to any of the components of the vaccine.
3. If you’ve reacted badly to a previous dose of the vaccine. The decision for the second round should be reached after a discussion with your doctor and a thorough clinical evaluation.
In case you’ve not been informed, the Gardasil manufacturer, Merck, has given you the right to report any negative side effects to the FDA by calling: 1-800-FDA-1088, or via the website: www.fda.gov/medwatch.
4. In a situation of moderate to severe illness, or high-grade fever, you are not a candidate for the vaccination till your health is restored as stated by the Centers for Disease Control and Prevention (CDC).
Kindly keep in touch by subscribing to our newsletter:
Functions of Gardasil vaccines.
Gardasil vaccines do not treat HPV infections. If you are already infected, taking it won’t cure you. Rather, it is meant strictly for prevention. Being infected with the human papillomavirus infection shouldn’t prevent you from getting vaccinated as it could still safeguard you from other strains of the virus you haven’t yet been exposed to.
There are up to 40 types of human papillomaviruses that infect the genital area and are considered to be either low or high-risk viruses as published by the US dept. Of Veteran Affairs Public Health article.
1. Low risk: These are known to be either harmless or responsible for genital warts and include HPV type 6 and type 11.
2. High risk: These are known to influence the regulators of the cell cycle, block tissue apoptosis, and induce abnormalities in cell chromosomes according to the Centers for Disease Control and Prevention (CDC). They are the oncoproteins that result in various cancers and include HPV types 16, 18, 31, 33, 45, 52, and 58.
In females, the vaccine prevents genital warts, and cancerous and precancerous lesions of the cervix, anus, neck, head, and oropharynx.
In males, it prevents genital warts, plus cancerous and precancerous lesions of the penis, head, neck, anus, and oropharyngeal tract.
The vaccines can achieve these because of the immunogenic VLP particles they contain which induce the body to produce antibodies that destroy human papillomavirus according to the National Cancer Institute (NCI).
These vaccines are highly effective however, they do not protect you against other sexually transmitted diseases according to the UK National Health Service (NHS) Having an HPV vaccine is not a license to be careless as there are other sexually transmitted infections one of which doesn’t have a cure Share on X
Gardasil vs Gardasil 9 and Cervarix.
In very simple terms, Cervarix (bivalent) is designed to protect you from two types of HPV infections (types 16 and 18) known to cause the majority of cervical cancers. Gardasil (Quadrivalent) is designed to protect you from four types of HPV viruses. That’s the two strains for which Cervarix offers protection plus two additional types (types 6 and 11) known to cause genital warts.
Above all, Gardasil 9 (nanovalent) protects you from all four types that Gardasil offers you protection from plus an additional 5 types of HPV (31, 33, 45, 52, 58) as shown in the table below.
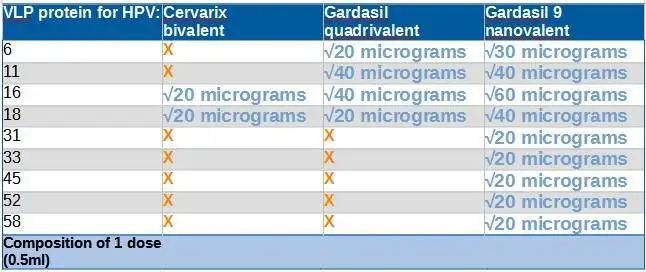
The table also shows the composition of a dose of each vaccine concerning the Virus-like particle content.
Please note that the current vaccines are for prophylaxis(prevention). So, if you are already infected with any of the viruses the vaccines can’t cure you. However, that doesn’t mean you can’t get vaccinated.
You’ll still need vaccination to protect you from other types of cancers or HP viruses you don’t yet have, as stated earlier. Nonetheless, efforts are being made to come up with one that could cure people of existing infections.
Vaccination recommended ages and schedules.
For prevention, the vaccines are most beneficial before people have been exposed to the papillomavirus and the best time is the preteen years. Below are the recommendations.
1. The Centers for Disease Control and Prevention (CDC) recommends that kids between the ages of 11 to 12 years be given 2 doses of the vaccine spread 6 to 12 months apart.
2. Two vaccine doses are deemed fit for all children below the age of 15 years or who haven’t had their 15th birthday before the first dose.
3. For those who have reached their 15th year of life and are between the ages of 15 – 26 years, three doses are recommended. 3 doses are generally recommended in the following circumstances:
- Children between 9-15 years who had their two doses less than 5 months apart.
- Children between 15 to 26 years.
- Kids between the ages of 9 to 26 years with weakened immunity.
4. The vaccines aren’t recommended for people above 26 years for the reason of being less beneficial due to exposure to HPV. they could still get immunized if they didn’t get the vaccine earlier or haven’t been well vaccinated. For them, it has to be 3 doses.
If you are between the ages of 15 to 45 years and billed for 3 doses, Gardasil manufacturer, Merck, recommends the second dose be given 2 months after the first and then the 3rd dose given 6 months after the 1st.
Generally, the age range for these vaccinations is 9 to 45 years.
The effectiveness of HPV vaccinations.
HPV vaccines have proven their efficacy since their approval in June 2006. They have led to a reduction in cases of cancer, genital warts, and precancerous lesions by over 80% according to the Centers for Disease Control and Prevention (CDC). The immunity conferred by these vaccines is safe and long-lasting, however, you can still get infected because the vaccines aren’t effective against all the strains of the human papillomaviruses there are and their overall effectiveness isn’t exactly 100%. At best, it could prevent more than 90% of all cancers attributed to HPV which to me is a good figure.
The UK National Health Service (NHS) has emphasized the need to complete the dosages for proper protection.
Side effects of Gardasil vaccines
Just as it is with almost all drugs, the HPV vaccines have known side effects that are neither serious nor life-threatening but could be determinants of your eligibility for the vaccination. Documented side effects include:
- Syncope.
- Nausea.
- Fever.
- Pain and soreness in the vaccination arm.
- Swelling.
- Joint and abdominal pain.
- Headache.
- Fatigue.
- Dizziness.
- Allergic reactions to any of the components of the vaccine.
Lying down to receive the vaccine and, or sitting for up to 15 minutes following vaccination helps reduce the chances of syncope and injuries that may result from a fall due to dizziness (CDC).
Parental concerns
According to the National Cancer Institute, studies have shown an increase in the number of parents declining to vaccinate their kids based on the vaccine’s safety. Almost twice as many parents declined in 2018 than in 2015.
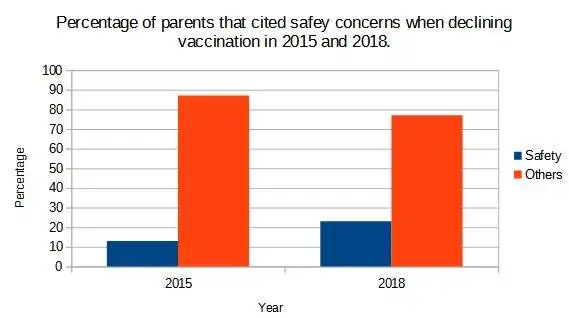
This is happening, despite the proven safety and efficacy of the vaccines, probably due to misinformation. Some of the unfortunate kids who didn’t get duly vaccinated may end up with diseases associated with the virus and also become sources of onward transmission of the infection to others.
To stem the tide, it was recommended that concerted efforts should be made to disseminate the right information to those who know better, especially health workers. Nonetheless, a recent study published in the New England Journal of Medicine (NEJM) suggests cancer vaccines should be further investigated.3
We figured out this could be news for parents who have concerns about cervical cancer vaccines and retweeted the information on X, which is one of our social media handles. You may want to join us there and give us a follow for more updates on the latest developments.
Vaccination cost
A dose of the Gardasil vaccine could cost up to $250 but there are ways of getting it at a very low cost or no out-of-pocket cost.
For instance, the vaccine manufacturer, Merck, runs a program by which uninsured US residents between 19 and 45 years old and with a certain household income could obtain it free. There are also some Federal programs put in place to get certain kids below 19 years vaccinated who meet the program’s eligibility requirements.
Insurance companies are also under a special mandate to cover the vaccination of children under the Federal Affordable Care Act as stated by the National Cancer Institute (NCI).
Treatment of HPV.
It’s great for mankind to have come up with a vaccine against HPV infection through vaccines that could tackle existing infections that are yet to be developed. Nevertheless, the future of the actual treatment of these infections looks bright with the discovery of an extract from a Japanese Mushroom.
The mushroom is called Shiitake and it’s a delicacy that’s native to many Asian countries. Clinical trials conducted by the University of Texas Health Science Center at the Houston Medical School, using an extract from this mushroom, showed significant success in the treatment of confirmed HPV infections.4
They used a compound called Active Hexos Correlated Compound (AHCC) extracted from shiitake for daily oral treatment of 10 women for 6 months. 5 of the participants at the time of the last available report from the center had tested negative for the virus. 3 participants showed full eradication after stopping the treatment while the remaining two were still undergoing treatment.
A study described in the National Library of Medicine was done to establish concrete treatment guidelines and showed a 60% efficacy in the elimination of the virus and persistent infections.

An Active Hexos Correlated Compound (AHCC) extracted from these mushrooms has been successfully used to treat HPV infections.
How to protect yourself from HPV if you can’t get vaccinated.
If for any reason you can’t get vaccinated there are steps you could take to protect yourself from the virus. They are simple and actionable plans to reduce your risk of exposure to the virus. These were well discussed in a previous article on the early stages of cervical cancer.
HPV is a major sexually transmitted disease. One way to avoid getting it is to avoid sex but telling anyone that is a fast-track means of making enemies and something tells me you’ll never agree to that.
Being more sexually discreet and sticking to a one-lifetime sex partner should come as better advice. However, the possibility of achieving that happens to be the next-door neighbor to zero in today’s society so we should be grateful to whoever invented condoms.
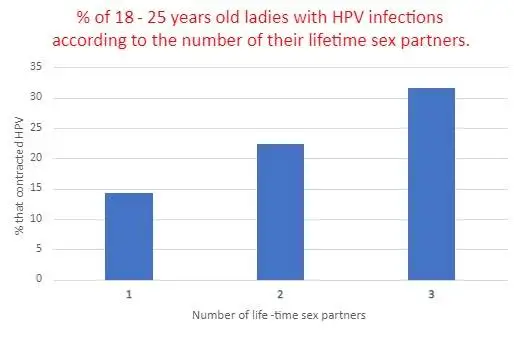
A study conducted on ladies between the ages of 18 and 25 years has shown a correlation between the number of lifetime sex partners and HPV infections.
Conclusion.
In conclusion, the HPV vaccine doesn’t take away your need to continue with cervical screening tests. Gardasil doesn’t protect everyone against HPV infections. It doesn’t protect against every HPV infection let alone other sexually transmitted diseases for which it wasn’t designed.
So, we all have personal roles to play in keeping fit and healthy irrespective of whether we are vaccinated or not.
The cervix is not the only part of the body women have cancer, breast cancer is common and has medically known symptoms you may want to read up and how breasts are reconstructed after mastectomy.
References.
- Cervantes, J. L., & Doan, A. H. (2018). Discrepancies in the evaluation of the safety of the human papillomavirus vaccine. MemóRias do Instituto Oswaldo Cruz, 113(8). https://doi.org/10.1590/0074-02760180063 ↩︎
- Frazer, I. H. (2019). The HPV Vaccine Story. ACS Pharmacology & Translational Science, 2(3), 210-212. https://doi.org/10.1021/acsptsci.9b00032 ↩︎
- Weber JS et al. Individualized neoantigen therapy mRNA-4157 (V940) plus pembrolizumab versus pembrolizumab monotherapy in resected melanoma (KEYNOTE-942): A randomized, phase 2b study. Lancet 2024 Jan 18; [e-pub]. (https://doi.org/10.1016/S0140-6736(23)02268-7. opens in new tab) ↩︎
- University of Texas Health Science Center at Houston. (2014, October 28). Mushroom extract, AHCC, helpful in treating HPV. ScienceDaily. Retrieved February 1, 2024 from www.sciencedaily.com/releases/2014/10/141028122424.htm ↩︎


























































































































I would like to thank you for the efforts you have put in writing this website. I am hoping the same high-grade blog post from you in the upcoming ones also. Actually your creative writing abilities has encouraged me and the blog is spreading its wings rapidly. Your write up is great.
I don’t usually comment but I gotta do that here for this great post.
It’s hard to find knowledgeable people on this topic, but you sound like you know what you’re talking about! Thanks