Table of Contents
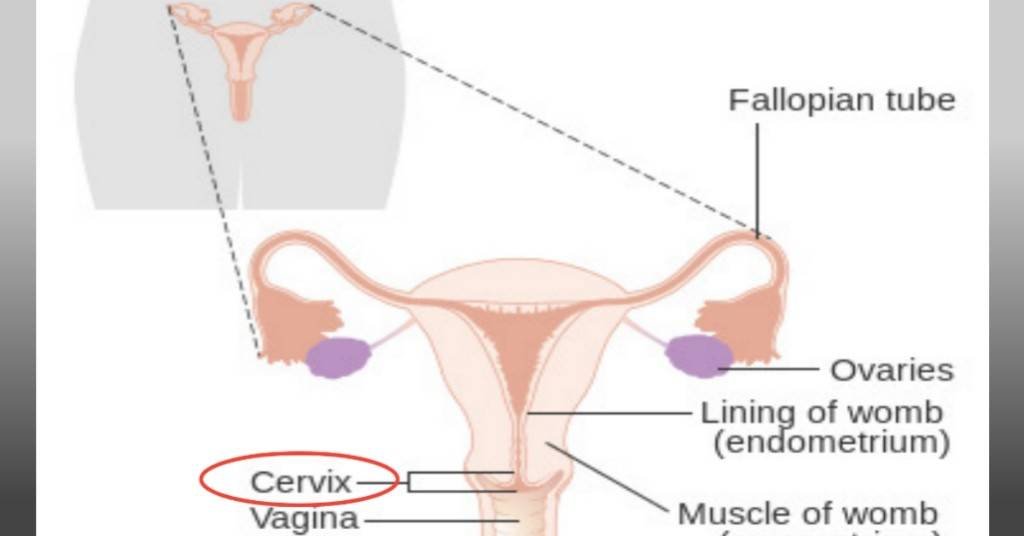
Appropriate treatment of cervical cancer is made possible by staging. It helps to accurately evaluate the spread of the disease, the type of cells where it started, and ultimately the best line of treatment. It is done with the use of a system called the International Federation of Gynecology and Obstetrics (FIGO).
In the FIGO system, the stages are numbered from 1 to 4 with 4 being the terminal stage whereas 1 is the earliest. These stages are each further divided into substages according to the extent of spread and size as shown in the table below.
| Stage | Sub-stage | Groups |
|---|---|---|
| 0. Precancerous. Abnormal growth of cervical cells. | – | – |
| —————— | ——————- | ————— |
| 1A. So small it’s seen with a microscope or colposcope. | 1A1. Less than 3mm deep. | |
| 1. Confined strictly within the cervix. | 1A2. Between 3-5mm deep. | |
| 1B. Comparatively bigger in size and area. | 1B1. More than 5mm but less than 2cm. | |
| 1B2. Up to 2cm but less than 4cm. | ||
| 1B3. Up to 4cm. | ||
| ———– | ———– | ———– |
| 2A. Cancer extended lower to reach the upper part of the vagina. | 2A1. Not more than 4cm. | |
| 2. Cancer has now extended beyond the cervix into surrounding tissues but not the lymph nodes or distant organs. | 2A2. More than 4cm. | |
| 2B. At this point, it has reached the tissues surrounding the cervix. | ||
| ————- | ———– | ———- |
| 3A. Cancerous cells have reached down the walls of the vagina but not the walls of the pelvis. | ||
| 3. Tumor has reached the lower parts of the vagina and possibly nearby lymph nodes but not distant organs. | 3B. It has now gone through the pelvic walls and, or blocked one or both of the tubes that drain urine(ureters). This results in kidney problems. | |
| 3C. The cancer is now seen to have reached nearby lymph nodes. | 3C1. Cancerous cells at this stage have reached nearby pelvic lymph nodes. | |
| 3C2. The cells have now gone up to extend to the para-aortic lymph nodes. | ||
| ———– | ————— | ————- |
| 4. At this stage cancer has finally reached other organs. | 4A. Cancerous cells have reached nearby tissues or organs like the bladder. | |
| 4B. At this later stage, it has spread to more distant organs and lymph nodes. |
In this article, we’ll take a look at the treatment for cervical cancer by stage beginning with tests carried out to determine what stage cancer has reached, at the time of diagnosis.
The tests that are used to determine the stages.
Cervical cancer cells spread either through lymphatic drainage, blood vessels, or direct proliferation into neighboring tissues. The more they spread, the further they take you down the stages. Your situation gets more precarious with increasing stage numbers.
Certain tests are done to determine the stage of the disease. They include:
- Cystoscopy. Find out if it has reached the urinary system.
- Laparoscopy. The use of an instrument called a laparoscope to check for the disease via an incision.
- Ultrasound. Uses sound waves to create images of internal organs on a screen.
- CT scan. (computerized tomography scan)
- Xrays. Checks the spread to the lungs
- MRI.(magnetic resonance imaging)
- PET scan. (Positron emission tomography scan)
- Biopsy. Checks for spread to the lymph nodes.
- Colposcopy. Used alongside a speculum for direct visual assessment.
- Intravenous Pyelogram (IVP)or Excretory urogram. For the examination of your urinary tract
- Proctosigmoidoscopy: The use of an instrument called a Sigmoidoscope to examine the Rectum for cancer cells.
- Blood tests.
Treatment for cervical cancer stage 1

For stage 1 cervical cancer surgery is the main treatment. There are a couple of surgical procedures and the type chosen for you depends on certain considerations. I discussed the treatment of stage 1 cervical cancer with a table on the types of surgeries for this stage of cancer in detail in a previous article you may want to read up.
Survival rate.
Up to 95% of people diagnosed with stage 1 cancer survive the next five years from the date of their diagnosis according to Cancer Research, UK.
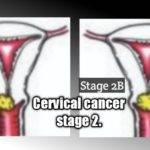
Treatment for cervical cancer stage 2
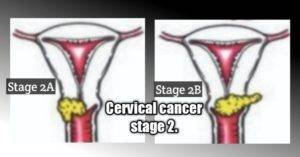
Chemoradiation is usually the preferred treatment choice for stage 2 as discussed in another article you may want to see titled the treatment for stage 2 cervical cancer. cervical cancer. However, there may be slight variations between the treatment choices for stage 2A and 2B cancers.
During chemoradiation, external beam radiation therapy(EBRT) is given once daily, 5 times weekly for about 5 weeks. During the treatment, chemotherapy is given once weekly or after every 2 to 3 weeks. This depends on the type of drug in use.
Your treatment course is then rounded off with internal beam radiation, called intracavitary brachytherapy which is a type of brachytherapy for stage 2 cervical cancer treatment as has been recommended by the Cancer Research, UK and Canadian Cancer Society.
For once-weekly chemotherapy, cisplatin may be the drug of choice for you, and for once every 3 weeks of chemo, cisplatin plus 5-fluorouracil may be administered.
Radical hysterectomy surgery may be done with pelvic lymph node dissection. Para-aortic lymph node sampling is also done to check for cancerous cells.
Chemoradiation may not be applicable in every case. For instance, in 2A, if no cancer cells were found near the edges of removed tissues or in the lymph nodes
Survival rate or life expectancy.
According to Cancer Research, UK 70% of women with stage 2 cervical cancer live for the next 5 years after detection of cancer. A pretty good figure, and with advances in medical research, it’s only going to get even better.
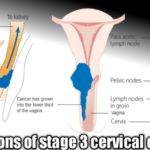
Treatment for cervical cancer stage 3
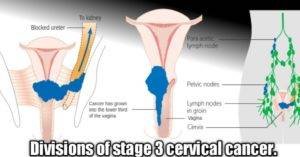
Just as in stage 2, chemoradiation has been recognized as the standard treatment for stage 3 cervical cancer as discussed in a previous article on the treatment for stage 3 cervical cancer. This involves a combination of radiation therapy and chemotherapy.
The procedure for the chemoradiation is just as described in stage 2 above.
3-dimensional conformal radiation therapy has been described which delivers targeted radiation specifically to the tumors in a way that spares surrounding tissues and organs from getting damaged by radiation as discussed in the Journal of the American Cancer Society.1
Studies have shown surgery to be another valid option for the treatment of stage 3 cervical cancer. However, there may still be a need for radiotherapy post-surgery to destroy any remaining cancer cells that may be missed during the surgery according to the American Cancer Society,2 and also suggested in the European Journal of Cancer.3
Survival rate or life expectancy.
According to Cancer Research, UK, more than 40% of sufferers live up to 5+ years from the date of initial diagnosis.
Keep in touch by signing up for our newsletter:
Treatment for cervical cancer stage 4
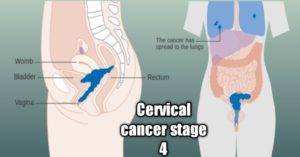
The particular treatment you receive at stage 4 cervical cancer is determined by the location of cancer in your body, the type of cells involved, and your state of health concerning the tolerance of the procedure according to Cancer Research, UK.
There are 4 options for your treatment which are:
1. Radiation therapy,
2. Chemotherapy,
3. Vascular endothelial growth factor (VEGF) targeted therapy,4
4. Surgery like a pelvic exenteration,5
Treatment choice is often a combination of any of the above 4 options like in Chemoradiotherapy.
The chemoradiation could involve the administration of about 25 doses of external Radiotherapy once daily for about 5 weeks (5 per week) and a course of chemotherapy weekly or once every 2 to 3 weeks according to Cancer Research, UK.
At the end of your treatment, you may be given internal radiotherapy which is also called Brachytherapy. This involves the use of radioactive materials to deliver doses of radiation targeting cancer directly. There are two types of Brachytherapy:
1. Temporary brachytherapy or High-Dose-Rate Brachytherapy (HDR): In this type, a radioactive seed is inserted close to the tumor to deliver high-dose radiation for about 10 to 15 minutes.
2. Permanent brachytherapy or Low-Dose-Rate Brachytherapy(LDR): This involves the permanent implantation of the radioactive seed in your body to keep delivering low-dose therapeutic radiation to the tumor. Its radioactivity wanes over time.
The American Brachytherapy Society recommends High-Dose-Rate brachytherapy for treating cervical cancer.6
In the European Journal of Surgical Oncology, primary exenteration has been described as a valid option for chemoradiation in the treatment of stage 4 cervical cancer, and secondary exenteration surgeries are recommended for recurrent cancers that remain confined within the pelvis.7
In an earlier article, you’ll find specific details on managing stage 4 cervical cancer according to its divisions.
Survival rate.
Only about 15% of people with this terminal stage of cervical cancer are known to live for the next 5 years from the date of diagnosis according to Cancer Research, UK. This is a far cry from an over 80% survival rate for people with early-stage cancer as stated in another article you may want to see titled cervical cancer early stage you may want to see.
Conclusion.
These treatments don’t guarantee survival. The best option open to all is to ensure you get appropriately vaccinated at the recommended ages and schedule the vaccinations. The vaccines that are presently available are purely for preventive measures but efforts are being made to make the ones that could also treat people already infected with the virus.
Meanwhile, the future of treatment of HPV infections is bright with the discovery of a Japanese mushroom called shiitake. Clinical trials done by the University of Texas Health Science Center have shown it has commendable curative properties.
References.
- Minn, A. Y., Hsu, A., La, T., Kunz, P., Fisher, G. A., Ford, J. M., Norton, J. A., Visser, B., Goodman, K. A., Koong, A. C., & Chang, D. T. (2010). Comparison of intensity-modulated radiotherapy and 3-dimensional conformal radiotherapy as adjuvant therapy for gastric cancer. Cancer, 116(16), 3943-3952. https://doi.org/10.1002/cncr.25246 ↩︎
- Panici, P. B., Scambia, G., Baiocchi, G., Greggi, S., Ragusa, G., Gallo, A., Conte, M., Battaglia, F., Laurelli, G., Rabitti, C., Capelli, A., & Mancuso, S. (1991). Neoadjuvant chemotherapy and radical surgery in locally advanced cervical cancer. Prognostic factors for response and survival. Cancer, 67(2), 372-379. https://doi.org/10.1002/1097-0142(19910115)67:2<372::AID-CNCR2820670210>3.0.CO;2-5 ↩︎
- Benedetti-Panici, P., Greggi, S., Scambia, G., Amoroso, M., Salerno, M., Maneschi, F., Cutillo, G., Paratore, M., Scorpiglione, N., & Mancuso, S. (1998). Long-term survival following neoadjuvant chemotherapy and radical surgery in locally advanced cervical cancer. European Journal of Cancer, 34(3), 341-346. https://doi.org/10.1016/S0959-8049(97)10029-6 ↩︎
- Magdalena Salomon-Pierzyńska, Beata Rembielak-Stawecka, Bogdan Michalski, Aleksander Perzyński, Violetta Skrzypulec-Plinta. (2014). VEGF – targeted therapy for the treatment of cervical cancer – literature review. Ginekologia Polska. Vol 85, No 6. DOI 10.17772/gp/1754. https://journals.viamedica.pl/ginekologia_polska/article/view/45878. ↩︎
- Brophy, P. F., Hoffman, J. P., & Eisenberg, B. L. (1994). The role of palliative pelvic exenteration. The American Journal of Surgery, 167(4), 386-390. https://doi.org/10.1016/0002-9610(94)90121-X ↩︎
- Nag, S., Erickson, B., Thomadsen, B., Orton, C., Demanes, J. D., & Petereit, D. (2000). The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix. International Journal of Radiation Oncology*Biology*Physics, 48(1), 201-211. https://doi.org/10.1016/S0360-3016(00)00497-1 ↩︎
- (2019). Palliative pelvic exenteration: A systematic review of patient-centered outcomes. European Journal of Surgical Oncology, 45(10), 1787-1795. https://doi.org/10.1016/j.ejso.2019.06.011 ↩︎