
Table of Contents
Infectious or septic knee arthritis is the infection of a knee joint’s synovial fluid and tissues by a bacterial, fungal, or viral infection. These often get to the joint via your blood, infected wounds, injections, or surgical procedures. Staphylococcus aureus bacteria is the cause of most septic knee arthritis.
Septic knee arthritis affects mostly children, people engaged in the use of illegal drugs, and the elderly. It has to be treated promptly to avoid irreversible complications.
Causes and risk factors.
Septic knee arthritis isn’t among the class of idiopathic diseases known to afflict man. It has definitive causes and risk factors.
Causes.
As stated earlier, the disease usually occurs as a result of infection. The infective pathogens could get to the joint from other parts of your body through the bloodstream or by a direct introduction via an open wound, surgery, or even an intra-articular injection.
According to the Journal of Clinical Microbiology and Infection, most times it occurs from bacterial infections by staphylococcus, streptococcus, Neisseria gonorrhea, Haemophilus influenza, gonococcus, mycobacteria, or viruses like HIV, hepatitis, and parvovirus. The Candida species of fungi like Candida albicans is not left out.
The risk factors.
Certain factors are known to place you at a greater risk of developing septic knee arthritis. These include:
Age: the disease is predominant in young people and the elderly.
Cancer: A study published in the Journal of the British Society for Rheumatology has shown septic arthritis can be a late complication of breast cancer.
Recent or past surgeries: People who have had past knee surgeries or surgeries done close to the knee joint could develop the disease.
Autoimmune diseases: The treatment of these diseases, like rheumatoid and psoriatic arthritis, involves the use of drugs that suppress the immune system. This makes you susceptible to septic arthritis from an infection.
Drug and alcohol abuse: Any of these two factors or in combination, as published in a scholarly review, is known to increase your risk of the disease.
Open wounds: Staphylococcus aureus, which is known to be the major cause of septic knee arthritis exists even on the skin of healthy individuals. Open wounds give it access into the body from which it could spread to the knee joint.
Immune-compromised patients: Patients or people with a compromised immune system are more likely to end up with the disease. This is because the body may not be able to adequately kill the causative pathogen in the event of an infection.
Presence of other joint diseases: The presence of other joint problems like lupus or osteoarthritis increases the risk.
AIDS or HIV: This is known to break down the body’s natural defenses against infection. In this way, they place you at increased risk of the disease.
The artificial knee joint: Knee prostheses are also a risk factor as supported in a Journal by the American College of Rheumatology.
Symptoms.
Symptoms associated with septic knee arthritis are typical of what you’ll expect during a fever and joint inflammation. The following symptoms are common:
- Swelling,
- Warmth,
- Pain,
- Chills,
- Redness,
- Tachycardia(raised heart rate),
- Reduced appetite.
- weakness and fatigue,
- Difficulty in ambulation or movement.
The pain experienced worsens with movement which makes normal movement of the knee joint difficult. Pain, warmth, swelling, and redness are all components of inflammation whereas chills, tachycardia, loss of appetite, weakness, and fatigue are common signs of fever. Fever is common during a systemic infection even in those that are not associated with septic knee arthritis.
Kindly keep in touch by subscribing to our newsletter:
Diagnosis.
The synovial fluid in the knee joint is usually sterile and functions as a lubricant. Investigation of this fluid is a crucial part of the tests used in the diagnosis of the disease. Below is a step-by-step procedure for the diagnosis:
- History taking: This helps to know what could be suspected. Someone whose history has one or several risk factors as outlined in the earlier part of this article may have your doctor suspecting septic arthritis. The more risk factors you have, the higher the probability of making a diagnosis of septic arthritis.
- Physical examination: After the history taking comes a physical exam. Your healthcare provider may check for some of the symptoms of the disease like warmth, pain, swelling, etc.
- Arthrocentesis: It is a crucial step during which a syringe is used to aspirate some synovial fluid. The sample of the fluid is sent to the lab to test for white blood cell count, and bacteria, among other things.
- Blood tests: This also helps to check for infection and the markers of inflammation.
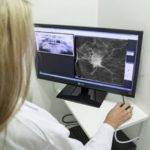
- Medical Imaging: It may be in the form of MRI, CT scans, or X-rays at a certain stage of the disease. This is used to check for joint damage.
Treatment.
The treatment is often started in the hospital on an in-patient basis which means you’ll have to be admitted. The ideal treatment for each individual depends on a couple of factors such as:
- The severity of septic knee arthritis,
- Your age,
- The predominant or most disturbing symptoms,
- Your state of health or the presence of any comorbidity.
The following are standard treatment plans but the exact procedure for yours may be modified after duly considering the above-listed determinants. This is to come up with a procedure that best suits you.
Joint aspiration and arthroscopy.
With the presence of infected fluid in the joint, no treatment will make sense without first draining the fluid. This can be done by aspirating the fluid with the use of a syringe and needle. At times arthroscopy-assisted joint irrigation and removal of infected matter become necessary.
There are times when multiple attempts at clearing the fluid have to be made as it accumulates after each clearance. Leaving a drain for continuous fluid clearance for a few days is also done when necessary.
Septic knee arthritis antibiotics.
Following the removal of infected fluid and matter from the joint, antibiotic or antifungal medications are commenced. The choice of antibiotics, as published in the National Library of Medicine, will depend on the result of a culture and sensitivity tests done to determine the actual pathogen and what drugs it’s sensitive to. Where this result isn’t available broad-spectrum antibiotics will have to be used.
With the right treatment, you could start feeling better within 2 days. The pains ease off as you take your non-steroidal anti-inflammatory drugs.
Unlike when we treat rheumatoid or psoriatic arthritis, glucocorticoids are not ideal when dealing with septic knee arthritis so are not encouraged as a scholarly study has shown.
We don’t treat viral-mediated septic knee arthritis like we do for arthritis of bacterial and fungal origin. Treatment of septic knee arthritis caused by viruses is normally symptomatic. By this, I mean we treat the symptoms. However, the use of anti-viral medications when dealing with HIV and hepatitis B or C, mediated arthritis, makes for quicker outcomes according to a scholarly study.
Septic arthritis knee and physiotherapy.
The physiotherapist helps to maintain, improve, or restore the muscle strength of the group of muscles that move the knees. They also help with the restoration of the functional range of movement of your knee joint apart from managing your pains and other aspects of inflammation.

Orthosis.
These are knee braces and splints that may be employed to help with your pains. They help by stabilizing and supporting the joint. Your physiotherapist or healthcare provider may recommend a suitable one.
Surgery.
The involvement of surgery is based on two criteria:
- Failure of the use of aspiration and arthroscopy to clear the infected fluid. Open surgery could then be carried out.
- Damage to the joint resulting from septic knee arthritis. The surgical options for this have already been described in a previous article.
Complications.
Septic knee arthritis requires a kind of urgent care as subchondral bone loss and permanent joint damage as a study has revealed can happen within 24-48 hours if the right antibiotic or antifungal drug isn’t started.
Septic knee arthritis ICD 10.
ICD stands for the International Classification of Diseases. ICD-10 was designed to aid in the measurement of treatment outcomes, making clinical decisions, enhancing data for research, uncovering fraud, making payment systems, etc. ICD codes for bacteria-induced arthritis for unspecified knee, right knee, and left knee are as shown in the table below.
| ICD-10 codes. | |
|---|---|
| M00861 | Arthritis due to other bacteria, right knee, right knee. |
| M00862 | Arthritis due to other bacteria on left knee. |
| M00869 | Arthritis due to other bacteria, unspecified knee. |
Nonetheless, there is an updated version, ICD-11, which was adopted in 2019 by the World Health Assembly but became effective last year on the 1st of Jan., 2022.
I hope this article was helpful. If there are other things you would like to know on this topic do let me know. Do have an awesome day and keep fit and healthy.


























































































































Oh my goodness! what an amazing article, dude. Thank you.