Table of Contents
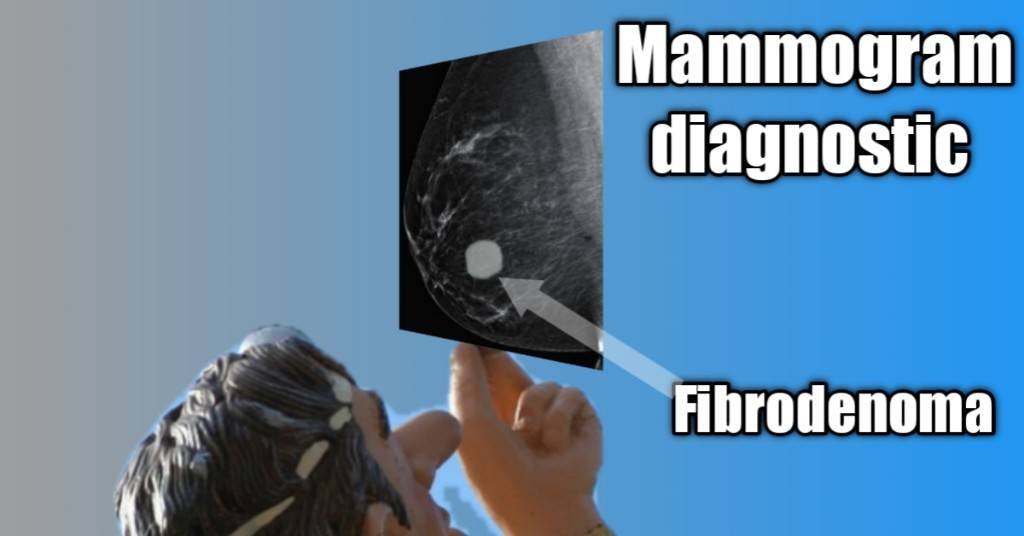
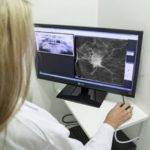
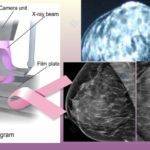
A Mammogram diagnostic is a Prescription-only measure meant to investigate abnormal developments in your breasts.
Unlike screening mammograms where you can refer yourself once you are above 40 years old, a diagnostic must be ordered by your physician when there are suspicious abnormal changes in your breasts.
Screening vs. diagnostic mammogram.

Whereas Screening mammograms are routine tests used to monitor your breasts for any abnormal changes, mammogram diagnostic is a next step test ordered when screening tests reveal the existence of abnormalities or when there are symptoms. These could be:
- Microcalcifications.
- Pain and inflammation.
- Discharge from the nipple.
- Tumor.
- Cysts.
- Pitting and dimpling on any side of your breast etc.
|
Screening Mammogram |
Diagnostic mammogram |
| First Step test | Next step test |
| Routine check | Prescription-only check |
| Less detailed | Much more detailed |
| Cheaper | Costlier |
| Takes less time | Takes more time |
| Fewer X-rays are taken | More X-rays are taken |
| No zooming required | Zooming of particular areas for clearer views |
| No point compression needed | Point compression of areas of suspicion |
| Done with no symptoms | Ordered because of symptoms |
Generally, diagnostic mammograms are ordered when the result of your screening shows suspicious abnormalities, or when you develop symptoms before your next scheduled screening.
Guidelines.
These are very much like what you do in preparation for your screening mammogram, such as:
- Book your mammogram with the nearest excellent center to you.
- Go along with any previous mammograms.
- Take with you the written order recommending you for it, if necessary.
- Don’t take caffeine or tea days to your test as they make your breasts tender.
- Wear a top you could take off easily rather than a gown.
- Endeavor to avoid using deodorants, powders, and perfumes on your appointment day.
- You may want to avoid the use of jewelry for convenience since you’ll have to take them off for the test.
Mammogram diagnostic procedure.
- Relate any concern you may have with the Radiologist or mammographer before the test.
- You’ll be asked to undress from the waist up and given suitable wear for the procedure.
- You then get to stand in front of the machine.
- Your breast is positioned on the machine’s lower plate.
- A plastic upper plate is lowered to compress your breast against the lower one. This compression is necessary to spread out your breast tissue so the low-dose X-ray used for the procedure could still obtain clear enough images.
- It also tends to eliminate blurring as it keeps the breast from moving during imaging.
- Unlike screening mammograms, mammogram diagnostic will involve taking many more images including spot compression or spot compression with the magnification of the areas under suspicion. This is done to obtain more detailed imaging of the abnormalities for which the diagnosis was ordered.
It is normal for you to feel some discomfort or even pain during the compression.
The pain usually resolves shortly and where it persists, it’s not expected to remain for more than a few days. If it does, you may have to talk to your doctor about it.
Your result.
Of the thousands of women who undergo mammogram diagnostic yearly, only a small fraction is diagnosed with cancer. Chances are the abnormalities for which you underwent diagnostic tests will turn out noncancerous.
So, you don’t have to freak out when you get a call back for a diagnostic mammogram following your routine screening.
According to the American Cancer Society (ACS), of all the women who undergo mammograms, less than 1 of every 10 who get a call back are diagnosed with breast cancer.
Your result might take a couple of days to be sent to your referring physician after which you’ll be duly informed.
Accuracy of your mammogram diagnostic results.
A publication in the National Library of Medicine has it that breast density and age tell a lot about the accuracy of a diagnostic mammogram. The older you are, the less dense your breasts are and therefore, the more accurate.1
Ultrasound does better for women below 45 years but it’s done in conjunction with mammograms as there are abnormalities ultrasound will usually miss, such as microcalcifications.
Diagnostic mammograms’ accuracy is over 83% in women above 50 years. The fattier the breasts, the more accurate, unlike the denser breasts in younger women.
Accuracy also depends on the technology employed (2-D or 3-D tomosynthesis), as contained in the National Library of Medicine (NLM)2 and American Journal of Roentgenology (AJR),3 and the level of experience of the Radiologist. This human equation persists even with experienced physicians.
Cost.
Owing to the extra work involved, detailing, and other factors, Mammogram diagnosis is expected to cost more than screening mammograms.
The National average cost if you are not on insurance is said to be about $499. You can expect the cost will vary with various test centers, locations, and states.
Billing and Coding.
Healthcare payers like Medicaid and Medicare do get volumes of billing to treat. For comprehensiveness and system efficiency they are sent in codes you may have come across.
Common among these are the CPT and ICD codes.
ICD-10-CM, which you may have heard, is the US clinical modification of World Health’s ICD-10. More information about it is available online.
CPT stands for Current Procedural Terminology and highlights the treatment being administered. ICD on the other hand stands for international classification of diseases and points to the reason for the treatment.
In 2017, the CPT took down the codes from 77051 to 77057 and introduced 3 new codes that included Computer-aided Detection (CAD). The new codes include 77065, 77066, and 77067.
77065- Diagnostic mammography, including CAD when performed, unilateral.
77066- Diagnostic mammography, including CAD when performed, bilateral.
77067- Screening mammography, bilateral (two-view study of each breast), including CAD when performed.
You’ll notice that the only screening mammogram is bilateral. If you are up for a unilateral screening mammogram, you are advised to check your payer guidelines for the reporting on a unilateral screening Share on X
A mastectomy of one breast may be a reason for a unilateral mammogram. The computer-aided detection, CAD, helps radiologists in the identification of abnormalities in your digital mammogram and was approved in 1998 by the Food and Drug Administration (FDA).
H2. Conclusion.
Getting an order for a mammogram diagnostic isn’t something that should get you worried. It’s just for additional and detailed investigation of suspected parts of your breast, or abnormalities.
The possibility of cancer being found after the screening is pretty low.
Mammograms are very effective in the diagnosis of cancers, particularly in older women as against younger women below 45 years.
Ultrasound which is often done in conjunction with mammograms improves the chances of detecting cancerous tumors but may also lead to higher false positives and avoidable biopsies.4 This is apart from detecting tumors that would have never caused you any harm if left alone.
Choice of test and follow-up procedure are things you’ll need to discuss with your doctor for the best advice and guidance to avoid overdiagnosis or over-treatments.
If there is something you are still not clear about in the context of this article, feel free to reach out to me.
References.
- Devolli-Disha, E., Manxhuka-Kërliu, S., Ymeri, H., & Kutllovci, A. (2009). COMPARATIVE ACCURACY OF MAMMOGRAPHY AND ULTRASOUND IN WOMEN WITH BREAST SYMPTOMS ACCORDING TO AGE AND BREAST DENSITY. Bosnian Journal of Basic Medical Sciences, 9(2), 131-136. https://doi.org/10.17305/bjbms.2009.2832 ↩︎
- Goldman, L. E., Walker, R., Miglioretti, D. L., Smith-Bindman, R., & Kerlikowske, K. (2010). Accuracy of Diagnostic Mammography at Facilities Serving Vulnerable Women. Medical Care, 49(1), 67. https://doi.org/10.1097/MLR.0b013e3181f380e0 ↩︎
- Leonard Berlin. (2007). Accuracy of Diagnostic Procedures: Has It Improved Over the Past Five Decades? American Journal of Roentgenology. Volume 188, Issue 5. https://doi.org/10.2214/AJR.06.127. ↩︎
- Berg WA, Blume JD, Cormack JB, et al. Combined Screening With Ultrasound and Mammography vs Mammography Alone in Women at Elevated Risk of Breast Cancer. JAMA. 2008;299(18):2151–2163. doi:10.1001/jama.299.18.2151 ↩︎


























































































































I don’t even know how I ended up right here, however, I found this submission to be very good. I do not know who you might be but definitely you are going to be a well-known blogger in case you are not already 😉 Cheers!