
Table of Contents
Breast reconstruction has a lot of positive social and psychological impacts to it. Though it seems to be about improving cosmetic appearances, it’s rather regarded as reconstructive surgery.
This article is focused on the reconstruction of breasts after cancer that was treated surgically.
Benefits of breast reconstruction.
Reconstructing your breast, as stated earlier may have psychosocial and physical benefits such as:
- Restores your positive perception of your body to some extent.
- Restores your confidence in your physical appearance.
- Keeps you from looking weird in certain clothes.
- Saves you the troubles of fixing and removing prosthetic breasts, daily.
- Reduces any negative impact of a mastectomy on your relationships.
- Staves off the negative impact of public glare if you were to move about with a flat chest.
Types of breast reconstruction.
There are two types of breast reconstruction. These are implant and autologous (flap) reconstructions.
Whichever type, could be placed in only one of two positions in the breast which is either above the chest muscle or below it.
Implant reconstruction.
Silicone and Saline implants are the two types of breast implants in use. They both have an outer layer made of a solid form of silicone but are distinguished by what this layer is filled with.
Silicone implants, it’s filled with silicone (a non-reactive and safe substance) whereas saline implants are filled with a sterile salt solution which is also safe.
Differences between saline and silicone Implants.
Though they are both contained in a silicone outer shell, there are notable differences between them as shown in the table below.
| Saline Implants | Silicone Implants |
|---|---|
| Costs less. | Costs more. |
| May feel rippled or wrinkled. | Feels more like natural breasts. |
| Feels heavier. | Feels lighter. |
| Can be used for 18 years and above. | Has a minimum age restriction of 22 years by the FDA. |
| Requires smaller incision. | Requires comparatively bigger incision. |
| Easier to notice when ruptured. | A rupture may go unnoticed till a mammogram is done. |
| Comes empty and filled after inserting it into the breast area. | It comes filled with silicone and has a definite size. |
| Easier to achieve symmetry with the opposite breast. | Achieving symmetry is more challenging. |
| Gets absorbed into the body after rupture. | Doesn’t get absorbed after rupture. |
| Doesn’t need an MRI. | Will need a regular MRI every 2 years to check for leakage. |
Autologous or flap reconstruction.
These are more invasive and complex procedures that often require microvascular surgeons (surgeons who specialize in the repair and union of blood vessels and nerves). They feel more natural than implants and involve the use of tissues obtained elsewhere in your body to create a breast.
These types of breast reconstructions follow two main surgical methods of transferring the tissues from donor sites to the breasts.
In the first and earlier method, the tissue remains attached to its natural anatomical blood supply. This is called a pedicle flap which may be taken from the abdominal wall (rectus abdomini) or latismuss dorsi. The flap is then moved under the skin to reach the breast area.
An improvement to that technique is the free flap. This is the second method.
It involves the complete excision of the needed tissue with its blood vessels from the donor site. It’s then used for breast reconstruction during which the tissue gets connected to a new blood supply by linking it with blood vessels around the breast.
Breast reconstruction by free flaps is complex, takes a longer time, and has to be done by a microvascular surgeon.
Flap breast reconstruction techniques are named according to the artery or part of the body the tissues are obtained from and include:
1. TRAM flap: Meaning Transverse Rectus Abdominal Myocutaneous flap. The skin, fat, and muscles from the lower abdomen are used for breast reconstruction.
2. DIEP flap: Stands for Deep Inferior Epigastric Perforator flap. Uses only the skin and subcutaneous fat from the lower abdomen thereby sparing the muscle.
3. LD flap: That is the Latismuss dorsi muscle flap. The skin, subcutaneous fat, and muscle in the back called the latismuss dorsi are used for this process.
Though it creates a natural-looking breast but may require an implant to make up for a deficiency in the volume of the reconstructed breast as the amount of tissue at the back is normally little.
4. SIEA flap: Superficial Inferior Epigastric Artery flap. Uses the skin, and fatty tissues under the skin plus a stomach wall artery called the inferior epigastric artery.
There is no risk of herniation as the muscles are left in place. No abdominal weakness as well and ideal for active people.
5. IGAP flap. Means Superior Gluteal Artery Perforator flap. Uses skin and subcutaneous fat tissues from the inferior part of the buttocks. Ideal for women with more subcutaneous fat at the gluteus and if the surgery fails it could be repeated with the opposite buttock. It’s great for very active women and women in sports.
6. SGAP flap. Superior Gluteal Artery Perforator flap. The skin and fatty tissues in this case are obtained from the superior part of the buttocks. Has similar characteristics to IGAP mentioned above.
7. PAP flap. Stands for Profunda Artery Perforator flap. It involves the use of the skin, subcutaneous fat, and blood vessels of the inner back part of your upper thigh. No muscle is lost but it leaves considerable scarring around the area.
8. TUG flap. Transverse Upper Gracili flap. This is similar to the PAP flap but involves a thigh muscle called the gracili. It’s cut from across the upper part of the inner thigh. There isn’t so much muscle weakness felt as the affected muscle isn’t among the critical ones.
9. DUG flap. Diagonal Upper Gracili flap. It’s quite similar to the TUG flap but in this case, the cut is made down the inner part of the thigh.

Image credit: Flickr
The American Cancer Society (ACS) has very good image descriptions of these surgeries. Below is a table compiled to give you a better overview of the different types of flap reconstruction.
| Reconstruction technique | Donor site | Advantages | Disadvantages |
|---|---|---|---|
| TRAM flap | Lower abdomen | 1. Natural-looking breasts. 2. Doesn’t need implant augmentation provided there is enough abdominal tissue for the surgery. | 1. Causes weakness of the area or donor site. 2. There is the risk of herniation or bulge, especially in very active people. 3. Leaves a scar at the donor site. |
| DIEP flap | Lower abdomen | 1. No abdominal weakness because the muscle is spared. 2. No risk of herniation or bulging at the donor site. 3. Good for very active people. | 1. More complex than TRAM and requires lengthier surgery time. 2. More prone to complications during the surgical process. 3. Leaves scar at the donor site. |
| LD flap | Back | No risk of herniation or bulge. | An implant is usually needed to make up for an expected deficiency in the volume of the reconstructed breast. |
| SIEA flap | Abdomen | 1. No resultant abdominal wall weakness. 2. No herniation can result. 3. Great for active people. | 1. The procedure has a higher risk of blood clots. 2. Not many women have sufficiently large blood vessels for it. |
| IGAP flap | Lower Buttocks | 1. No risk of organ herniation, bulge, or muscle weakness. 2. Surgery can be repeated if the previous one fails. | 1. Can create asymmetrical buttocks. 2. The procedure is complex and prone to complications. 3. Scarring at the donor site. |
| SGAP flap | Upper buttocks | 1. No risk of organ herniation, bulge, or muscle weakness. 2. Surgery can be repeated if the previous one fails. | 1. Can create asymmetrical buttocks. 2. The procedure is complex and prone to complications. 3. Scarring at the donor site. |
| PAP flap | Back part of the upper thigh. | Not associated with muscle weakness. | 1. Scarring at the crease of thigh and buttocks. 2. A complex procedure that can result in complications. |
| TUG flap | Across the upper part of the inner thigh. | A non-successful surgery can be repeated using the contralateral (opposite) leg as the donor site. | 1. Associated with muscle weakness. 2. Scarring. |
| DUG flap | Down the upper part of the inner thigh. | A non-successful surgery can be repeated using the contralateral (opposite) leg as the donor site. | 1. Associated with muscle weakness. 2. Scarring. |
You may wonder how the implants are held in place within the location of the breasts. This is made possible with the help of a hammock created with an acellular dermal matrix sourced from a human or pig’s skin. according to a Biomaterials Journal.1
The dermal matrix used has been processed and sterilized to clear all cells that could trigger tissue rejection and infections as recommended by the National Cancer Institute (NCI).
Timing of your reconstruction surgery.
Should you decide to have breast reconstruction surgery, there are two options open to you concerning when it should be done. These are:
- Immediate reconstruction: Usually carried out at the same time as your mastectomy or started after the mastectomy.
- Delayed reconstruction: Done months or years after mastectomy.
Which of the two you end up doing is a decision you’ll need to make from discussing with your doctors who are trained to guide you into making the right one. The following factors are known to influence that decision.
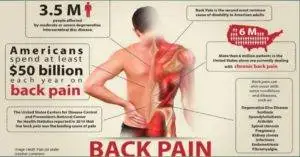
1. Radiation therapy. This is the most important factor in determining the appropriate timing for your reconstruction. The presence of implants could interfere with the delivery of radiation to target areas.
This could affect the efficacy of your treatment but having the reconstruction done before radiation (which could mean immediate reconstruction when possible) is better as the procedure may be problematic after radiation.
For anyone having natural tissue reconstruction but must go through radiation, a delayed reconstruction is better. This arrangement enables the damaged body tissues from the radiation to be replaced by healthy ones during the reconstruction.
In the absence of radiation therapy, flap tissue reconstruction could still be done immediately following mastectomy with great outcomes as a study in the Journal of American Society of Plastic Surgeons has revealed.2
2. Type of cancer. Cancers associated with inflammation may result in extensive loss of the skin of the breast from a mastectomy. For there to be a reconstruction there has to be tissue expansion.
Since tissue expansion isn’t ideal after radiation, it implies immediate reconstruction may be the way to go for those billed for radiation since neither the expansion nor insertion of the implant is ideal after radiation.
Choosing the best for your situation is something to discuss with your doctor.
3. Amount of breast skin spared. If there is sufficient breast skin left it’s an indication for immediate reconstruction which can be done at the same time as the mastectomy.
4. Type of reconstruction. If you are billed for post-mastectomy radiation therapy, autologous (tissue flap) reconstruction is best if delayed till after the adjuvant therapy whereas reconstruction involving breast implants may be better before radiation and where possible done immediately.
Whichever time a reconstruction using implants is done, some complications could result from radiation.
5. Personal choice. You usually have the choice to decide when you want your reconstruction done. You may want to have it delayed even if you are a candidate for immediate reconstruction or choose not to have any at all.
Nipple and areola reconstruction.
The nipple is an essential part of a normal breast without which the breast can’t be said to be complete. There is nipple-sparing mastectomy and it’s possible when the location of the cancer allows it.
However, if you lost your nipple and areola during the mastectomy it is possible to have it reconstructed to improve the overall appearance of your breasts. This procedure is carried out after you have healed or recovered from the breast reconstruction.
It’s achieved by using bits of skin cut from the reconstructed breast to create a nipple as shown in the video above. The areola can be surgically created a few months later with skin grafts from the groin, or stomach, or by drawing a 3D tattoo of it around the nipple.
If you had to go through radiotherapy after mastectomy, surgical nipple construction may be a bad idea owing to the effects of the radiation on soft tissues. In your case and for anyone who doesn’t want a surgical nipple reconstruction, a 3-D tattoo will do.
How to prepare for the surgery.
1. You’ll do well to stop smoking if you smoke as it delays healing and increases risks.
2. Do the research and look for a reputable microvascular or plastic surgeon with experience.
3. Write down all the questions you may have and ask all you want to know about your surgery.
4. Join support groups in your locality or online to learn from others’ experiences.
5. Discuss your hopes for the surgery to help align your expectations with realities.
6. If you are on any medications, bring them to the notice of your surgeons.
7. You may be asked to stop herbal supplements, anti-inflammatory drugs, and blood thinners (anticoagulants and antiplatelet drugs) in due time.
8. Depending on your unique situation, certain medications may be prescribed, and some tests.
9. Avail yourself of any help offered by family, friends, and people who have been in your situation.
10. Before your surgery, find out what you’ll need at home that will be helpful in your recovery.
The outcome of your surgery and expectations.
It’ll take a while to see the outcome of your surgery but most importantly, having realistic expectations is key to your overall satisfaction.
There are things your breast reconstruction can achieve and those it can’t. Learning all you can about it even before your surgery goes a long way in streamlining your hopes with realities.
The look and feel of reconstructed breasts vary among individuals. The kind of adjuvant therapy given will also greatly impact the outcome and in most cases may have a long-term effect if it happens to be radiation therapy according to the International Journal of Radiation Oncology.3
As mentioned earlier in this article, with your breast reconstruction the contour of a breast shape is restored so you don’t end up with a flat chest. This makes your clothes fit better, keeps you from looking weird publicly, and reduces the social and psychological impact of a mastectomy.
With the reconstruction, some self-confidence in your physical appearance is restored, however, the breast can’t look and feel exactly like the natural one that was removed. There will be a loss of sensation post-op that may improve over time, in some cases. The surgical scars will also fade but will never go away completely.
Some risks and complications may result and will need further surgery to address or physical therapy to manage.
If your reconstruction was on one breast, achieving some level of symmetry may mean carrying out some surgical procedures on the contralateral (opposite) breast. However, reconstruction with an implant will result in greater asymmetry as the opposite breast changes with aging.
Whatever your experience in the long and short term, always bear in mind that the most important goal in your treatment is to ensure the breast cancer doesn’t return. As long as that is achieved and the cancer doesn’t come back, that should give you reasons to smile and be happy.
Comparison of flap and implant reconstructions.
Tissue flaps and implant-based breast reconstructions each have their unique advantages over the others. Below is how they compare, on some key points of interest.
| Flap tissue reconstruction | Implant reconstruction |
|---|---|
| Doesn’t rupture. | Can rupture, requiring another surgery. |
| Prone to more complications. | Has fewer complications if done without radiation therapy. |
| Involves two surgical sites. | Involves one surgical site. |
| Leaves two surgical scars. One at the donor site and the other at the breast. | Usually leaves one scar which is at the breast. |
| Has a longer recovery time. | Has a shorter recovery time. |
| May feel more natural than implants. | feels comparatively less natural. |
| Requires more surgical procedures. | Requires fewer surgical procedures. |
| Has a longer period of surgery especially free flaps. | Has a shorter period of surgery. |
| The breast size will change accordingly if you gain or loss weight. | The breast size is static and may look smaller if you gain weight. |

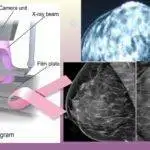
Mammograms after breast reconstruction?
You normally aren’t expected to carry on with mammograms on a breast that has had a mastectomy but what if it was only on one breast? That means you’ll have to continue with your mammogram screenings as scheduled, on the other breast.
Having an implant reconstruction after mastectomy should exempt you from having a mammogram of that affected breast but what if it was an autologous (flap tissue) reconstruction coupled with having had a skin-sparing mastectomy?
To ensure you remain safe from cancer I believe you will agree with the call to continue mammograms on the reconstructed breast.
The National Cancer Institute (NCI) believes that being at high risk of breast cancer should mean having a mammogram of a reconstructed breast if it was done using flap tissues from other parts of your body.
Summarily, having an autologous breast reconstruction surgery after mastectomy may mean continuing with mammography in certain circumstances Share on X.
Risks and complications of breast reconstruction.
Every surgery is associated with risks and is only considered expedient where the benefits outweigh the risks. In that same vein, breast reconstruction has known risks some of which are:
1. Infections. Infections are common in surgeries and are often accompanied by undue or heightened pains as contained in the European Journal of Surgical Oncology. Getting it treated as soon as possible is important to avoid complications associated with it.
Radiation therapy is known to increase the risk of infections in breast reconstruction as proven in research published in Researchgate.4
2. Necrosis. It’s the death of tissues within the breast and could occur when the blood supply to transplanted tissues in autologous breast reconstruction is compromised especially in free flap tissue reconstruction.
If the microsurgery to connect the free flap to a blood supply isn’t properly done, necrosis of the tissue is inevitable.
Smoking could also increase the chances of necrosis as it narrows blood vessels thereby reducing the availability of nutrients and oxygen to tissues used for breast reconstruction.
3. Delayed healing. Several factors could result in the incisions not healing within the expected time which will prolong the period of wound care. Some of these are infections, effects of radiation, and smoking as stated in the American Journal of Medicine.5
4. Soft tissue contractures. This distorts the shape of implants, causes pain, and may need surgical intervention in some cases. Some women do have a latismuss dorsi flap reconstruction where an implant is used to augment the size of the breast.
For these women, the formation of contractures could make mammography painful if they are billed to continue with mammograms after reconstruction.
5. lingering pains. Apart from contractures that may form around implants, calcium deposits could also build up around implants and both of these developments are known to cause pain and could be the reasons for another surgery.
6. Tissue stiffness or tightness. It could come as a direct result of radiation as adjuvant therapy and may have to be managed for a long time with physical therapy.
7. Effect of anesthesia. For this reason, you may not be able to do certain things by yourself for a while like driving yourself home after the operation. Make an arrangement to be driven home after your surgery, instead.
8. Blood clot. It could be a problem in flap tissue reconstruction.
9. Permanent numbness. Surgery involves cutting of nerves and this leads to the loss of sensation or numbness. It could get better with time but there’ll still be areas of numbness.
10. Implant rupture. Implants are built to last but ruptures do happen and could have you go in for another surgery. Silicone implant rupture usually goes unnoticed but the impact of a rupture on saline implants soon becomes obvious due to asymmetry.
11. Breast asymmetry. Reconstructed breasts could differ from the other breast by any measure creating a noticeable asymmetry between the two breasts especially if you had a silicone implant.
12. Scars. With bodily injuries, scars could form, and surgical incisions are like injuries to normal skin. The scars reduce with time but never actually go away.
13. Herniation of abdominal organ. When the muscle is included in a tissue flap obtained from the abdominal wall, it leaves behind an area of weakness through which herniation could occur in very active people.
14. Muscle weakness. Muscle groups that act as donor sites for autologous reconstruction could have a noticeable weakness.
15. Repeat surgeries. Having had a breast reconstruction makes repeat surgeries almost inevitable, in some patients, many years down the line or within weeks or months from the time of reconstruction. They are usually done in response to complications.
16. Implant extrusion. Implants could break through the skin to the exterior. This is a surgical emergency that could lead to other complications like infection.
The best reconstruction after mastectomy.
As we’ve seen, there are several choices available to you when it comes to breast reconstruction. It’s not a one-size-fits-all. The decision on the particular type that best suits you should come after a conversation with your doctor.
Some of the factors that will determine the type of breast reconstruction you should have include:
1. Type of adjuvant therapy recommended: radiation therapy could result in a lot of complications if you are to have it before or after an implant. An autologous or flap tissue surgery may be a better option. It’ll also serve as a privilege to replace some of the tissues damaged by radiation.
2. Activity level: If you are into sports or are a very active person, this could be a factor in the decision-making process. You may want to avoid a TRAM flap reconstruction or any method that will lead to considerable muscle weakness.
3. Availability of tissue: The availability of enough skin and muscle to cover an implant could make you a candidate for immediate implant reconstruction.
4. Past surgery on donor site: Having a history of surgery on a donor site like the abdomen could mean opting for other methods.
5. Social habits: If you are in the habit of smoking, avoiding more invasive processes should be considered because of the effects of smoking on healing and recovery. You’ll already be asked to stop smoking weeks before your surgery anyway.
6. Size of the breast for reconstruction: Whereas smaller breast sizes can be reconstructed with tissues from donor sites that lack thickness like the Latismuss dorsi (LD flap) bigger breasts will demand areas with adequate tissue.
Do keep in touch by signing up for our newsletter:
Implants can also be combined with flap tissues to increase the volume of a reconstructed breast for purposes of symmetry.
7. Medical History: Certain medical conditions like diabetes could be a reason to opt for less invasive measures owing to their effect on wound healing and recovery.
8. Your preferences: Above all, your personal preferences are always considered and could be a strong deciding factor in the type of reconstruction you get. What’s the use of a great technique if you don’t derive joy in it?
One bad review from a single patient could translate to the loss of several patients to other facilities and no hospital wants that. It’s nightmarish.
By and large, if you are billed for radiation therapy, autologous tissue reconstruction is something I’ll advocate as suggested in the European Journal of Surgical Oncology.
How long your surgery may take?
With enabling conditions, some breast reconstructions could happen at the same time as your mastectomy. Should there be a need for tissue expansion it could take a couple of months of regular appointments to gain enough tissue size that could cover an implant.
In other words, a need for tissue expansion could tremendously increase the time it’ll take to complete your entire reconstruction process. Having to reconstruct either one or both breasts will also impact the timing in as much as the type of planned reconstruction (that is if it’s an implant or flap reconstruction).
Depending on the reconstruction method that applies to you, it could take between 3 to 12 hours including the preparation.
Recovery and pain management.
You may be discharged with pain medications in about 3 to 5 days after surgery, depending on the type you had. There may be a drain in place which you’ll be taught how to empty before your discharge. It’s meant to drain fluid from surgical sites while they heal.


It’s normal to feel weak and sore for about 2 to 3 weeks. Limit activities and lifting for 4 to 6 weeks post-surgery during which you won’t be expected to engage in certain exercises like stretching. Swelling and soreness should’ve gone down in 6 to 8 weeks.
It may take up to 8 to 9 weeks before you can return to work and normal life. Please be patient.
After a level of healing, report to your doctor if you start having symptoms like tissue discoloration, pain, lumps, discharge from surgical sites, or swelling.
The American Cancer Society (ACS) recommends physical therapy to help you regain some level of function post-op.
It may take up to 1 to 2 years for you to feel quite healed but research carried out on about 4,000 women that have undergone breast surgeries has revealed there may be lingering pains up to 2 years after surgery. This is due to unavoidable tissue and nerve damage incurred during the operation.
Mastectomy for some women may have ended regular mammogram screenings but breast reconstruction effectively replaces that with annual appointments with your plastic surgeon. This is aimed at monitoring the new breast for any developments, and of course, your doctor is your best friend even if mammography isn’t.
I hope this was helpful. You may check out a related post on breast biopsy with excision.
Reference.
- Chen, R., Ho, H., Tsai, Y., & Sheu, M. (2004). Process development of an acellular dermal matrix (ADM) for biomedical applications. Biomaterials, 25(13), 2679-2686. https://doi.org/10.1016/j.biomaterials.2003.09.070 ↩︎
- Xue, D., Qian, C., Yang, L., & Wang, X. (2012). Risk factors for surgical site infections after breast surgery: A systematic review and meta-analysis. European Journal of Surgical Oncology (EJSO), 38(5), 375-381. https://doi.org/10.1016/j.ejso.2012.02.179 ↩︎
- Pierce, S. M., Recht, A., Lingos, T. I., Abner, A., Vicini, F., Silver, B., Herzog, A., & Harris, J. R. (1991). Long-term radiation complications following conservative surgery (CS) and radiation therapy (RT) in patients with early-stage breast cancer. International Journal of Radiation Oncology*Biology*Physics, 23(5), 915-923. https://doi.org/10.1016/0360-3016(92)90895-O ↩︎
- Nahabedian, Maurice & Tsangaris, Theodore & Momen, Bahram & Manson, Paul. (2003). Infectious Complications Following Breast Reconstruction with Expanders and Implants. Plastic and reconstructive surgery. 112. 467-76. 10.1097/01.PRS.0000070727.02992.54. ↩︎
- Silverstein, P. (1992). Smoking and wound healing. The American Journal of Medicine, 93(1), S22-S24. https://doi.org/10.1016/0002-9343(92)90623-J ↩︎



























































































































Thanks for a great piece of information.
Some truly nice on this internet site, I like it.