Table of Contents
Cancers are usually named after where they originated irrespective of where they may have spread to before or after diagnosis. It’s the fourth most common cancer in women according to the World Health Organization (WHO).
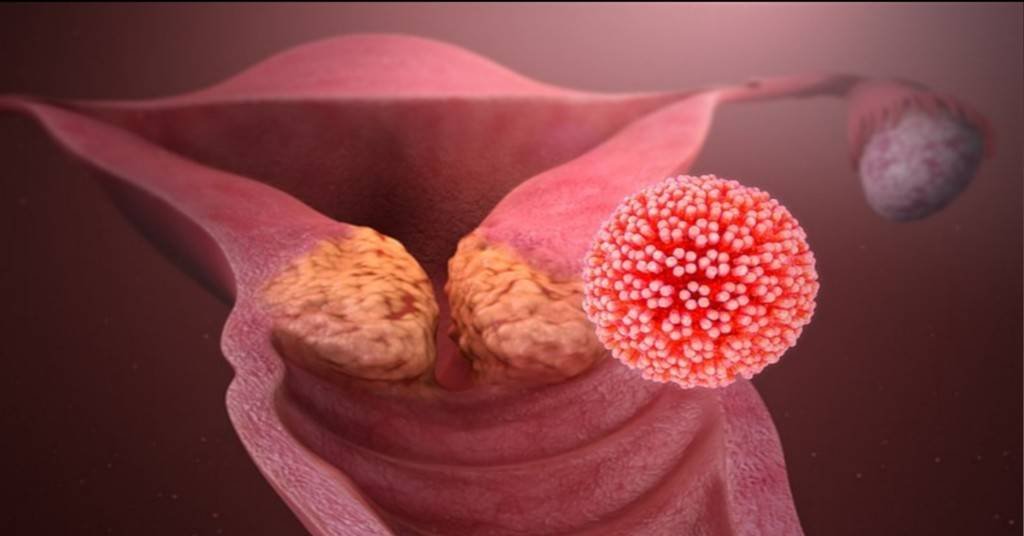
Cervical cancers are cancers that originated at the cervix, which is the neck of the womb that links it to the vagina. It’s mostly triggered by prolonged infection with the human papillomavirus (HPV).
Based on the International Federation of Obstetrics and Gynecology (FIGO) staging system, early stages of cervical cancers refer to stages 1A, 1B, and 2A. These stages may be symptom-less but later stages may be marked by abnormal vaginal bleeding, painful intercourse, and foul-smelling vaginal discharges.
In this article, we’ll take a look at cervical cancer’s early stage and other points of interest associated with it.
The development of cervical cancer.
It starts with cervical dysplasia which is the abnormal growth of cervical cells often triggered by a human papillomavirus infection. This is called the Precancerous stage which eventually leads to cervical cancer when not treated.
There are 3 levels of progressive Cervical dysplasia:
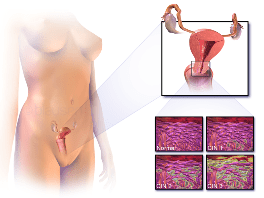
Image credit:
Blausen M.C inc.
- Mild dysplasia (CIN I)
- Moderate to marked dysplasia (CIN II)
- Severe dysplasia to carcinoma in situ (CIN III)
(CIN means Cervical Intraepithelial Neoplasia)
Cervical cancer occurs mostly in younger women below 44 years and it grows slowly. So slow that chances of early detection are high in women who get screened regularly.
According to the World Health Organization, it takes 15-20 years for cervical cancer to develop if your immunity is OK but as little as 5-10 years with weakened immunity occasioned by diseases like HIV.
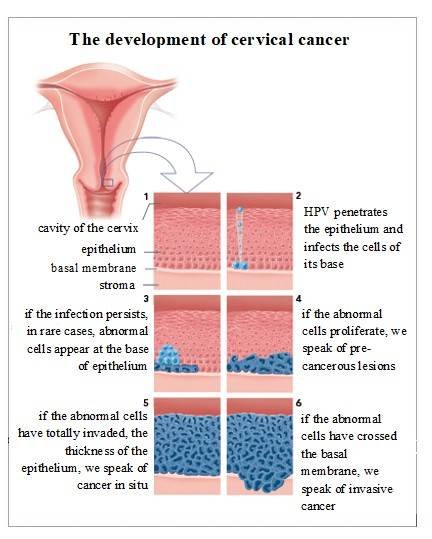
The process takes many years as mentioned earlier. It starts with the penetration of the cervical epithelium tissue by the Human Papillomavirus to infect the cells at its base as shown in the image below. From that point, abnormal cells appear in the base of the cervical epithelium in rare cases.
The proliferation of these abnormal cells at the base of the epithelium is described as precancerous lesions. Cancer in situ describes the situation where these abnormal cells have proliferated or invaded the thickness of the epithelium. Invasive cervical cancer refers to the situation when abnormal cells have crossed the basal membrane of the epithelium.
Types and symptoms.
Types
Two main distinct types make up the bulk of cervical cancers, which are named after the cells that turn cancerous, plus a couple of rare types. These are:
- Squamous cell carcinoma of the cervix. This forms the vast majority of cervical cancer cases (70-80%) and could be recurrent, according to the International Journal of Radiation Oncology The squamous cells affected are found in the outer parts of the cervix otherwise called the Exocervix. 1
- Adenocarcinoma. This starts in the mucus-producing gland cells of the inner lining of the cervix called the endocervix. Though the incidence is only a small fraction of that of squamous cell carcinoma it’s becoming more common. It constitutes about 20% of cases of cervical cancers according to Cancer Research, UK (CRUK).
- Adenosquamous carcinoma. As the name suggests, it’s a mix of the two previously mentioned two and makes up about 5-6% of cervical cancer cases.
- Small cell cancers. This is a rare type of cervical cancer. It makes up about 3% of the number of cases but is known to grow or progress much quicker than the more common ones as has also been described by the Cancer Research, UK.
Symptoms
Unlike breast cancer where the affected organ is visible and can be felt for abnormalities, you can’t see your cervix directly but there are symptoms associated with cervical cancer. Early stages are usually symptomless but the general symptoms associated with cervical cancer include:
- Bleeding after coitus(That’s after sexual intercourse).
- Bleeding between your periods.
- Post-menopausal bleeding.
- Foul-smelling watery, pale, pink, bloody, or brown-colored vaginal discharge, as has also been described by the government’s information on public health.
- Lower abdominal Pains. Often felt during sex, between your hip bones or lower back as also mentioned by the UK National Health Service (NHS).
As it spreads you may feel nausea, bone pain, physical fatigue, diarrhea, swollen legs, and difficulty passing out urine.
causes and risk factors.
Cancers happen when normally healthy cells start dividing without control, causing an unhealthy build-up of these abnormal cells to form a tumor. The same applies to cervical cells in the process leading up to cancer.
Causes.
There are over 100 types of the human papillomavirus (HPV) in existence and 14 of these are known to cause different kinds of cancers afflicting mankind according to the World Health Organization (WHO).
According to the World Health Organization, two out of the 14 cancer-causing types of HPV are known to trigger cervical dysplasia that results in cervical cancer. These are the HPV-16 and HPV-18.
Together, they are believed to be responsible for over 70% of all cases of cervical cancer according to the World Health Organization (WHO). HPV infections are common and usually transmitted via sex or skin contact.
Most people will contact them at a point in life but they usually clear out on their own. It’s when they linger that problems result.

Image credit: Scientific Animations
Risk factors.
Certain factors could increase your chances of having cervical cancer. A study published in the International Journal of Cancer has revealed the following risk factors:2
1. Weak body immunity: most HPV infections are taken care of by your immune system within 2 years. Having a compromised immunity will reduce your body’s chances of fighting off the infection.
2. Early sexual experience. That is becoming sexually active too early in life. A reason for mothers opposed to preteen vaccinations to reconsider their positions. Apart from the problem of juvenile delinquency, you can’t keep a tab on your child’s activities 24/7.
When something erupts, parents are the last most children will tell.
3. Smoking.
4. Multiple sexual partners.
5. Presence of STDs (sexually transmitted diseases).
6. Use of oral contraceptive pills.
7. Low educational status. This may surprise you but it’s true for several reasons.
8. Early age of first pregnancy.
9. Social class. It’s related to educational status according to the International Journal of Cancer.3
10. HPV infection. This is the main culprit and comes after a repeated or persistent HPV infection according to the World Health Organisation (WHO).
Most of these factors are interrelated. For instance, decreasing social class could result in sexual behaviors that predispose one to HPV, poor or no access to healthcare, and untreated infections leading to higher chances of having untreated precancerous stages.
This could eventually result in cervical cancer.
Early stages of cervical cancer.
Cervical cancer staging is necessary for the evaluation of the disease spread, and the determination of the most appropriate line of treatment. It is done with the use of a system called the International Federation of Gynecology and Obstetrics (FIGO).
It’s a 4 stage system based on clinical evaluation. Lower numbers are indications of non or less spread which means better treatment outcomes whereas higher figures represent more metastatic disease stages therefore poorer prognosis.
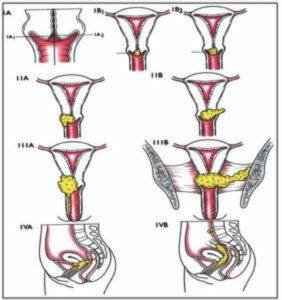
Image credit: Edna Maite Mohuba et al
The early stage we’ll cover here is stage 1 which has a couple of sub-stages.
Stage1
The cancer is limited to the cervix and has neither spread to nearby lymph nodes nor distant tissues. It has a couple of sub-stages such as:
1A sub-stage.
The cancer is so small that it’s only visible under a microscope or colposcope. This is further divided into two groups.
1A1: The cancer is still confined within the cervix and hasn’t penetrated deeper than 3mm into cervical tissues.
1A2: Here, the cancerous tissues are still only within the cervix but have gone deeper into the tissues up to a range of between 3-5mm deep.
1B sub-stage.
Though the cancerous cells remain restricted to the cervix, they are now bigger in size and area they occupy. There are three groups of 1B and they are defined by the depth of the cancer cells in the tissues of the cervix.
1B1: Deeper than 5mm but less than 2cm.
1B2: Up to 2cm deep but less than 4cm.
1B3: It’s up to 4cm deep.
The common characteristic of stage 1 is that cancer hasn’t left the cervix but varies in depth. This is about the safest time to treat it.
Though the early stage is central to this article, there exist three other stages as shown in the Table below. From the precancerous stage 0, the higher the number, the worse the expected treatment outcome, and the lower the average survivability.
| Stage | Sub-stage | Groups |
|---|---|---|
| 0. Precancerous. Abnormal growth of cervical cells | —- | —- |
| ———– | ——————— | ————— |
| 1. Confined strictly within the cervix. | 1A. So small it’s seen with a microscope or colposcope. | 1A1. Less than 3mm deep. 1A2. Between 3-5mm deep |
| 1B. Comparatively bigger in size and area. | 1B1. More than 5mm but less than 2cm. 1B2. Up to 2cm but less than 4 cm. 1B3. Up to 4 cm. | |
| —————- | ——————— | —————- |
| 2. Cancer has now extended beyond the cervix into surrounding tissues but not the lymph nodes or distant organs. | 2A. Cancer extended lower to reach the upper part of your vagina. | 2A1. Not more than 4 cm. 2A2. More than 4 cm. |
| 2B. At this point, it has reached the tissues surrounding the cervix. | ||
| ———————- | ———————- | —————- |
| 3A. Cancerous cells have reached down the walls of the vagina but not the walls of the pelvis. | ||
| 3. Tumor has reached the lower parts of the vagina and possibly nearby lymph nodes but not distant organs. | 3B. It has now gone through the pelvic walls and, or blocking one or both tubes that drain urine(ureters). This results in kidney problems. | |
| 3C. The cancer is now seen to have reached nearby lymph nodes. | 3C1. Cancerous cells at this stage have reached nearby pelvic lymph nodes. 3C2. The cells have now gone up to extend to the para-aortic lymph nodes. | |
| —————– | ———————– | ————— |
| 4. At this stage, the cancer has finally reached other organs. | 4A. Cancerous cells are found to have reached nearby tissues or organs, like the bladder. | |
| 4B. At this later stage, it has spread to more distant organs and lymph nodes. |
You’ll find more details about the stages of cervical cancer with very descriptive images from Cancer Research UK.
Screening and diagnosis.
Just as mammography serves for the screening of breasts for cancer as covered in a previous article, Pap smear tests (named after the inventor, Georgios Papanikolaou) are also used to screen for the presence of precancerous lesions that could result in cervical cancer. It’s a veteran test that has been in use as far back as 1940, probably long before you were born.
Below is a step-by-step descriptive video of Pap and HPV testing.
A second screening test that can be done in isolation or along with the pap test is the High-risk HPV testing. The United States Preventive Services Task Force (USPSTF) has recommended age-dependent guidelines for these tests as shown in the table below.
| Age. | Screening recommendations. |
|---|---|
| Less than 21 years. | Screening is not recommended. |
| 21-29 years. | Pap smear test (cervical cytology) every 3 years. |
| 30-65 years. | 1. Pap smear test every 3 years, or 2. High-risk HPV test (hrHPV) every 5 years, or, 3. Pap smear plus hrHPV every 5 years. |
| Above 65 years. | No testing if you’ve had a good screening record and are not at high risk. |
A biopsy is indicated if your screening tests come out positive. This is a process of taking a small tissue sample from the area for lab investigation. At times the sample taken could be in the shape of a cone in which case we call it a cone biopsy.
Other diagnostic tests like the following could follow the biopsy:
- Magnetic resonance imaging (MRI) test.
- Ultrasonography of the pelvis.
- Colposcopy. Used alongside a speculum for direct visual assessment.
- Computed Tomography (CT) scan.
- Blood tests.
- Intravenous Pyelogram (IVP)or Excretory urogram. For the examination of your urinary tract.
- Chest Xray. To check for spread to the lungs.
- Positron Emission Tomography (PET) scan.
- Proctosigmoidoscopy: The use of an instrument called a Sigmoidoscope to examine the Rectum.
Diagnostic tests provide data for the staging of cervical cancer and treatment plans. CLICK TO TWEET
Early-stage treatments.
Early-stage means the cancer is still confined within the cervix or hasn’t spread so much as shown in the table above. This makes it easier to treat with a good prognosis.
Surgery has proven to be very effective at ending the scourge of cervical cancer at this stage. Sometimes it may be combined with adjuvant therapies like radiation or chemotherapy for greater effectiveness.
You could spend an additional 2 days on admission after surgery for close monitoring. Healing could take up to 6 weeks.
Various types of surgery exist for the treatment of cervical cancer from the precancerous stage to the advanced metastatic stage. These include:
Cryosurgery: Involves the freezing of cancerous cells. A study contained in the American Journal of Obstetrics and Gynecology found this effective in the treatment of cancer cells that are still on the surface.5 It can also be used for the treatment of precancerous lesions.
Hysterectomy(or radical hysterectomy): Describes the total removal of an entire uterus with the cervix. This is an option in the later stages of the disease and will usually involve other measures due to the spread. It is associated with cure rates of over 80% according to the New England Journal of Medicine (NEJM).6
Pelvic exenteration surgery is an aggressive surgical procedure that tackles the advanced stages of cervical cancer as also contained in the Journal of Gynecologic Oncology.7 The Uterus, cervix, vagina, lymph nodes, and rectum gets removed and at times a part of the colon may be taken out as well.
Trachelectomy: This procedure spares the uterus thereby retaining your ability to have children as also covered in the International Journal of Obstetric and Gynaecology.8
Do keep in touch by subscribing to our newsletter:
Survival.
Detection and treatment of precancerous stage(0) are close to a 100% survival rate. I haven’t conducted any research to come up with survival rates but I’ll give two interesting statistics obtained from the American Cancer Society and Cancer Research, UK.
The calculations are based on the patient’s ability to live out the next 5 years from the time of initial diagnosis.
Based on the FIGO stages:
| FIGO stage. | 5-year survival rate. |
|---|---|
| Stage 1 | 95% |
| Stage 2 | 70% |
| Stage 3 | 40% |
| Stage 4 | 15% |
From Table 3 you’ll find the average survival rate for stages 1 and 2 is over 80%. This underscores the need for regular screening so cancer can be detected early.
The table below is the 5-year survival rate based on the extent of metastasis or spread:
| Extent of Metastasis | 5-year survival rate. |
|---|---|
| Local | 92% |
| Regional | 58% |
| Distant | 17% |
Prevention.
Vaccination is one surefire means of preventing the scourge. The Centers for Disease Control and Prevention (CDC) recommends vaccination for people between the ages of 9-12 years.

Image credit: Whispyhistory
People above 26 years don’t need vaccination unless they were not vaccinated before they became teenagers or didn’t complete their vaccination dose. On this note, vaccination can be administered for people aged 27 to 45 who failed to get enough vaccination while younger.
Other measures you could take that lower your chances of contracting the disease are:
- Regular Screening. Could detect precancerous stage. The treatment of this stage prevents the disease.
- Use of condoms. Condoms keep you safe from infections including HPV.
- Quitting smoking. Smoking compromises your immunity putting you at risk of the disease.
- Keeping to one sexual partner. Multiple partners increase your chances of contracting it.
- Early pregnancy. Avoid getting pregnant too early. Teenage pregnancy for instance.
Conclusion.
The major cause of cervical cancer is a virus transmitted mostly via sex. In other words, the HPV virus is sexually transmitted just like HIV. The good thing is that it is treatable even after contraction, unlike HIV.
Nonetheless, the prevention of any disease is always better than its cure. From what has been discussed, you can see staying safe from the virus isn’t rocket science and could save you from the loss of vital reproductive or sexual organs that make you whole as an individual.
This is cervical cancer month, let’s use it as a reminder of things we must do to keep safe from the disease. You may also want to see the topic of breast cancer or implants.
References.
- Hong, J., Tsai, C., Lai, C., Chang, T., Wang, C., Chou, H., Lee, S. P., & Hsueh, S. (2004). Recurrent squamous cell carcinoma of cervix after definitive radiotherapy. International Journal of Radiation Oncology*Biology*Physics, 60(1), 249-257. https://doi.org/10.1016/j.ijrobp.2004.02.044 ↩︎
- Bosch, F. X., Muñoz, N., Izarzugaza, I., Gili, M., Viladiu, P., Tormo, M. J., Moreo, P., Ascunce, N., Gonzalez, L. C., Tafur, L., Kaldor, J. M., Guerrero, E., Aristizabal, N., Santamaria, M., De Ruiz, P. A., & Shah, K. (1992). Risk factors for cervical cancer in Colombia and Spain. International Journal of Cancer, 52(5), 750-758. https://doi.org/10.1002/ijc.2910520514 ↩︎
- Parikh, S., Brennan, P., & Boffetta, P. (2003). Meta-analysis of social inequality and the risk of cervical cancer. International Journal of Cancer, 105(5), 687-691. https://doi.org/10.1002/ijc.11141 ↩︎
- US Preventive Services Task Force. Screening for Cervical Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(7):674–686. doi:10.1001/jama.2018.10897 ↩︎
- Popkin, D. R., Scali, V., & Ahmed, M. (1978). Cryosurgery for the treatment of cervical intraepithelial neoplasia. American Journal of Obstetrics and Gynecology, 130(5), 551-554. https://doi.org/10.1016/0002-9378(78)90074-1 ↩︎
- Alexander Melamed, M.D., M.P.H., Daniel J. Margul, M.D., Ph.D., Ling Chen, M.D, M.P.H., Nancy L.Keating, M.D., M.P.H., Marcela G. del Carmen, M.D., M.P.H., Junhua Yang, M.S., Brandon-Luke L.Seagle, M.D., Amy Alexander, M.D., Emma L. Barber, M.D., Laurel W. Rice, M.D., Jason D. Wright, M.D., Masha Kocherginsky, Ph.D., et al. (2018). Survival after Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer. New England Journal of Medicine. N Engl J Med; 379:1905-1914. DOI: 10.1056/NEJMoa1804923 ↩︎
- Schmidt, A., Imesch, P., Fink, D., & Egger, H. (2012). Indications and long-term clinical outcomes in 282 patients with pelvic exenteration for advanced or recurrent cervical cancer. Gynecologic Oncology, 125(3), 604-609. https://doi.org/10.1016/j.ygyno.2012.03.001 ↩︎
- Shepherd, J. H., F. Crawford, R. A., & Oram, D. H. (1998). Radical trachelectomy: A way to preserve fertility in the treatment of early cervical cancer. BJOG: An International Journal of Obstetrics & Gynaecology, 105(8), 912-916. https://doi.org/10.1111/j.1471-0528.1998.tb10238.x ↩︎


























































































































Good write-up, I am a normal visitor to your blog, maintain the nice work going on here, and i’m going to be a regular visitor for a long time.
Good one!
I think this site has some real superb information for everyone.
I will right away grab your rss as I can not find your e-mail subscription link or newsletter service. Do you have any? Kindly let me know so that I cab subscribe. Thanks.