
Table of Contents
Hemiplegia is a Greek word that consists of two components, Hemi and plegia. Hemi means one-half, and plegia represents paralysis. Together, they mean the paralysis of one half of the body. It is a non-progressive condition that usually happens as a result of an injury or lesion to the brain or spinal cord.
The clinical presentation of a hemiplegic patient will depend on the part of the brain affected or the spinal cord level, and the extent of the injury. There can be either left or right hemiplegia.
The brain consists of two parts, named the left and the right hemispheres. The nerve fibers from these hemispheres cross paths below the brainstem to supply the opposite sides of the body. This is called decussation. As a result, the left hemisphere supplies and controls the right side of your body, and the right hemisphere supplies the left side of your body.
So, left hemiplegia occurs when the right hemisphere of a person’s brain suffers a lesion or injury, while right hemiplegia happens when the lesion is in the left hemisphere. Hemiplegia resulting from spinal cord injuries (SCI) will usually affect the same side of the body as the injury (ipsilaterally). This is in contrast to brain injuries, where paralysis happens on the opposite side of the body (contralaterally).
Research1 National Library of Medicine. (governmental authority) Visit source has shown that left hemispheric stroke not only happens to be more common than the right one but also has the worse outcome. Share on X
Complete paralysis, aptly described by the term hemiplegia, has other clinical presentations in line with the part of the central nervous system affected. This also determines what part of the body goes into paralysis. In other words, it’s not always hemiplegia. There can be:
- Monoplegia: This is paralysis that affects just one limb, like a hand or leg.
- Paraplegia: Describes the paralysis of both lower limbs and is often seen in spinal cord injuries.
- Hemiplegia: This affects one side of the body, as I described earlier.
- Quadriplegia: Refers to paralysis of all four limbs as seen in spinal cord lesions occurring at the neck.
Types.
Hemiplegia can be broadly divided into two types based on the time of onset, namely congenital or acquired.
- Congenital hemiplegia is that which dates before the birth of a child, during delivery, or within the first 2 years after birth as a result of injury to the brain. It is a form of cerebral palsy in children, but with hemiplegic features.2 National Library of Medicine. (governmental authority) Visit source and can be regarded as unilateral cerebral palsy.
- Acquired hemiplegia, on the other hand, refers to paralysis that happens at any other time within the lifespan of a person after the first 2 years of life.
You may also group hemiplegia based on clinical features, area of the body affected, or pattern of attack. By this, we may have the following:
- Spinal hemiplegia: It is caused by a lesion along the course of the spinal cord and results in paralysis of one side of the body but hemianesthesia (loss of normal sensation) on the opposite side. This uncommon condition is also called Brown-Sequard syndrome.3 National Institute of Health. (governmental authority) visit source
- Contralateral hemiplegia: The more common type of hemiplegia, where a lesion in any of the brain’s two hemispheres results in the paralysis of the opposite side of the body.
- Facial hemiplegia: In this case, one side of the face gets paralyzed, resulting in facial asymmetry. It can occur alone or in association with paralysis of other areas of one’s body.
- Spastic hemiplegia: This is hemiplegia that is associated with the hypertonicity of muscles. The muscle tone is higher than normal, and the joints of the affected limb(s) feel slightly or markedly resistant to passive movements. You get this in lesions that occur within the brain and/or spinal cords of adults or children.
- Alternating hemiplegia: It is a disorder that affects kids who are below the age of 18 months.4 National Institute of Health. (governmental authority) Visit source . It may come when the child is awake, but goes into full remission when asleep. More about this will be discussed in the next section.

Alternating hemiplegia.
Alternating hemiplegia: This mostly occurs as a result of mutations in the ATP1A3 gene and, at times, also in the ATP1A2 gene, which reduces the activity of an enzyme called Na+/K+ ATPase. This enzyme affects the signals controlling muscle movement.5 National Institute of Health. (governmental authority) visit source
As stated earlier, it’s a rare disorder that starts in children who are mostly below the age of 18 months.6 Alternating hemiplegia. (scholarly source) visit source They experience episodes of paralysis on single or multiple limbs, and one half(hemiplegia) or both sides of their body.
It could be a brief or prolonged attack lasting days and could affect different parts of the child’s body at different episodes. When it affects both sides of a child’s body, it’s called bilateral hemiplegia or quadriplegia.7 Wikipedia: Alternating hemiplegia of childhood. visit source
Forms or categories of alternating hemiplegia
Alternating hemiplegia could be benign or serious.
- Benign nocturnal alternating hemiplegia of childhood (BNAHC): This is known for its good prognosis as it doesn’t lead to any known intellectual or neurological impairment.8 National Library of Medicine.(governmental authority) visit source
- Severe alternating hemiplegia: This is a more serious form that often leads to progressive intellectual impairments and dependence.
The episodes of hemiplegia occur throughout life9 MedlinePlus. (governmental authority) Visit source , but sometimes may become less severe after the child has lived beyond 10 years.10Wikipedia: Alternating hemiplegia of childhood. Visit source The attacks are usually triggered by conditions such as
- Cold,
- Stress,
- Tiredness, or
- Bathing.
Symptoms
The symptoms are either paroxysmal or non-paroxysmal:
- Paroxysmal: These are on-and-off symptoms that occur on their own or may accompany AHC attacks like epilepsy and dystonia. They may resolve at any time and are not permanent.
- Non-paroxysmal: These are permanent symptoms that don’t go away but may rather progress with time. You may describe them as side effects or complications of alternating hemiplegia of the child, like cognitive and intellectual decline, developmental delays, and ataxia (impaired coordination and balance).

Dense and flaccid hemiplegia.
Dense hemiplegia occurs in lesions involving the internal capsule of the brain, which may lead to severe paralysis of one-half of the body. This is because the internal capsule is a pathway that connects nerves controlling sensory and motor functions in your body, where these nerves are condensed within a relatively small area.
So, a small injury or lesion in the internal capsule can lead to marked paralytic symptoms and loss of sensation with a significant risk of the development of spasticity. Spasticity is clinically felt as hypertonia (abnormally high muscle tone) or stiff muscles, and it plays a major role in the development of bodily deformities.
Spasticity is usually preceded by flaccidity, which presents with weak muscles or poor muscle tone (hypotonia) following a stroke. Flaccid hemiplegia or paralysis is often temporary and present at the initial stages of a cerebrovascular accident (CVA). In one study, it was found to last for one or several months.11 Jamanetwork. (scholarly source) visit source
How to distinguish hemiplegia from hemiparesis.
Hemiplegia and hemiparesis are often used interchangeably, but there is a distinct difference between them.
Hemiparesis refers to weakness experienced in one side of the body as a result of brain or nerve injury. Paresis stands for weakness, while hemi denotes one-half of a whole. Someone with hemiparesis can still move affected limbs but experiences reduced muscle strength such that he or she expends more energy carrying out what used to be easy tasks.
Plegia, on the other hand, stands for paralysis rather than weakness. So hemiplegia means paralysis of one side of the body. Affected limbs usually can’t be moved or used even with enormous efforts.
A single injury may elicit both conditions at different times. In cases of stroke, the loss of function usually transitions from hemiparesis to hemiplegia, and during recovery or remission, it goes from hemiplegia back to hemiparesis.
A typical mild to moderate brain or nerve injury will elicit paresis or hemiparesis, whereas moderate to severe injuries result in hemiplegia. However, there are cases where it is difficult to distinguish the clinical presentation of the two, such as mild hemiplegia and severe hemiparesis.
Causes of hemiplegia.
Stay in touch by signing up for our newsletter:
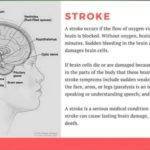
1. Cerebrovascular Accidents or stroke: This results from an interruption in the blood supply to parts of the brain, leading to varying degrees of cell death. It accounts for most cases of hemiplegia.
2. Traumatic brain injuries: Any accident where the head gets hit can result in damage to the brain. Such damage could lead to hemiplegia if one side of the brain is damaged, or even worse, if both sides are damaged.
3. Infections: It includes all infections leading to meningitis or encephalitis. Though bacterial infections are often the culprit, fungal and viral brain infections leading to hemiplegia are also common.
4. Demyelinating diseases: These are diseases that cause damage to the protective myelin sheaths that cover nerve fibers, like in multiple sclerosis. The sheaths play critical roles in the conduction of nerve impulses or signals. When damaged, there will be problems with the conduction of nerve impulses, leading to neurological conditions that may manifest as hemiplegia.
5. Sickle cell anemia: This isn’t so common, but I’ve handled a couple of cases arising from complications of sickle cell anemia, like vaso-occlusive disorders or ischemia that result in hemiplegia in sickle cell patients.12 National Library of Medicine.(scholarly source) visit source (cited July 9th, 2022)
6. Congenital hemiplegia: As described earlier, it is hemiplegia that occurs from birth or within the first 2 years of a child’s life and can be due to various causes.
7. Neoplastic: Refers to both cancerous and non-cancerous growths in the brain. Though cancerous cells from breast cancer or cervical cancer can give rise to hemiplegic symptoms when they spread to the brain, the situation isn’t regarded as brain cancer since the cells didn’t originate within the brain.
8. Brown-Sequard syndrome: Describes a type of spinal cord injury leading to hemiplegia. Unlike in cerebrovascular accidents, this type of hemiplegia occurs on the same side of the body as the damage. However, the opposite side of the body experiences a loss of temperature and pain sensations.
9. Genetic mutations: For instance, the mutation in the ATP1A3 gene. It is a rare condition that usually starts in childhood before the age of 18 months and continues throughout life.
A recent study published by the New England Journal of Medicine (NEJM) suggests that stroke or hemiplegia of whatever cause has declined statistically. However, for reasons that need to be discovered and addressed, it is more prevalent among the black population than the white.
- We discussed this finding on one of our social media handles, which you may wish to see. You may also want to follow us on our different social media channels for more updates. Just scroll down to the footer of this page and click to join us on the social media network(s) that work best for you.
Symptoms.
They could change over time, but some common symptoms you would expect in a stroke case include:
- Inability to move or use the limbs on the affected side due to paralysis.
- Facial deviation to the unaffected side.
- Inability to stand unsupported.
- Weak and flaccid muscles at some point.
- Spastic muscles.
- Loss of sensation or patchy sensation in some people.
- Loss of proprioception.
- Fecal and urinary incontinence.
- Cognitive decline.
- Difficulty in speaking or understanding others.
- Muscle wasting or atrophy.
- Growth discrepancy between the affected and unaffected sides in children.
- Difficulty eating or swallowing in some patients.
Note that not all of these symptoms are present in every stroke patient.
I listed additional physical, social, and psychological effects or symptoms of hemiplegia in an answer to a question on Quora13 What other effects might a stroke that results in left hemiplegia have? ( questions and answers site) Visit the site. So you may want to check it out.
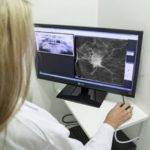
Diagnosis.

There are several medical tests employed in the diagnosis of hemiplegia. These include:
- Magnetic resonance imaging (MRI),
- Computerized tomography scan (CT),
- Full blood count (FBC), otherwise called Complete blood count (CPC),
- X-rays,
- Myelography,
- Electromyography (EMG).
Depending on the health facility, available equipment, and a couple of other exigencies, you may find that not all of these tests will be deemed necessary or ordered. However, among the most common ones in use are MRI, CT scan, and blood counts.
When hemiplegia is due to hypertension, a cardiologist may bring on board additional tests like the
- Electrocardiography (ECG or EKG),
- Echocardiography (Echo).
They are not meant to diagnose hemiplegia but to assist in the treatment of a hypertensive patient.
Treatment.
The first line of treatment and the most important of all is to address the underlying causative factor or condition and then stabilize the patient. For instance, a hypertensive patient will need to get the BP controlled as soon as possible and stabilized before other measures.
Otherwise, nothing else may work, and the patient will only deteriorate with time rather than improve. If a hemiplegic patient also presents with diabetes, making sure the blood sugar levels are well controlled within safe ranges is also important.
Surgical intervention may become necessary in the treatment of ischemic or hemorrhagic stroke. The aim is usually to remove the embolus or thrombus in cases of ischemia and to stop the bleeding in cases of hemorrhage. It may also be to prevent hemorrhage where there are physical factors that place patients at risk of it.
Some of the surgical interventions for the prevention of hemorrhage or the stopping of bleeding were described under the medical or emergency treatment for hemorrhagic stroke. However, research has been ongoing on surgical intervention for the treatment of stroke in the field of brain-computer interfaces (BCI).
Brain-computer interface intervention involves the surgical implantation of neurotech devices designed to pick up a stroke patient’s brain signals and thoughts. These signals are processed by a computer and then converted to physical functions through an output device.
Stroke treatment is generally a multidisciplinary approach, just like in many other medical conditions, but by far the bulk of the efforts towards restoration of functions and independent living lie in the hands of physical and occupational therapists.
The physical therapist engages you in extensive but repetitive exercises, which include:
- Passive Exercises,
- Assisted Exercises,
- Auto-assisted Exercises,
- Passive stretching,
- Kegel’s exercises (for incontinence)
- Resistance Exercises,
- Frenkel’s exercises,
- Other balance and coordination exercises in addition to Frenkel’s,
- Soft tissue mobilization (STM),
- Tactile stimulation,
- Modified constraint-induced movement therapy (mCIMT)14Journal of Physical Therapy Science. (scholarly source) visit source (cited July 10th, 2022),
- Electrical stimulation.

These processes help to induce neuroplasticity, which is essential in regaining lost functions and improving muscle strength, usability, and reliability.
In some cases, there may be a need for mobility aids and adaptive equipment, which may be temporary or permanent depending on the level of recovery.
Complications.
The complications of hemiplegia are closely related to the effects that were listed earlier, such as:
- Retarded limb growths in children that lead to discrepancies,
- Muscular atrophy,
- Incontinence,
- Spasticity,
- Soft tissue contractures,
- Joint stiffness, etc.
Prevention.
There are so many possible causes of hemiplegia that make prevention difficult. One can only be careful to avoid accidents that could result in spinal cord injuries (SCI) and traumatic brain injuries (TBI) that lead to it.
Managing what predisposes you to it, like high blood pressure is also key. This is in addition to getting babies promptly treated when they have a fever because high body temperatures can lead to brain injuries in infants, which could result in cerebral palsy.
If you are a sickle cell disease patient or a carrier, it is important that you marry or make babies with a partner who doesn’t have the disease. This is to avoid having babies with SS. This will require not marrying a carrier or a fellow sickler. As mentioned earlier, sickled red blood cells could result in vaso-occlusive disorders that can cause hemiplegia.


























































































































Some superb information.