Table of Contents
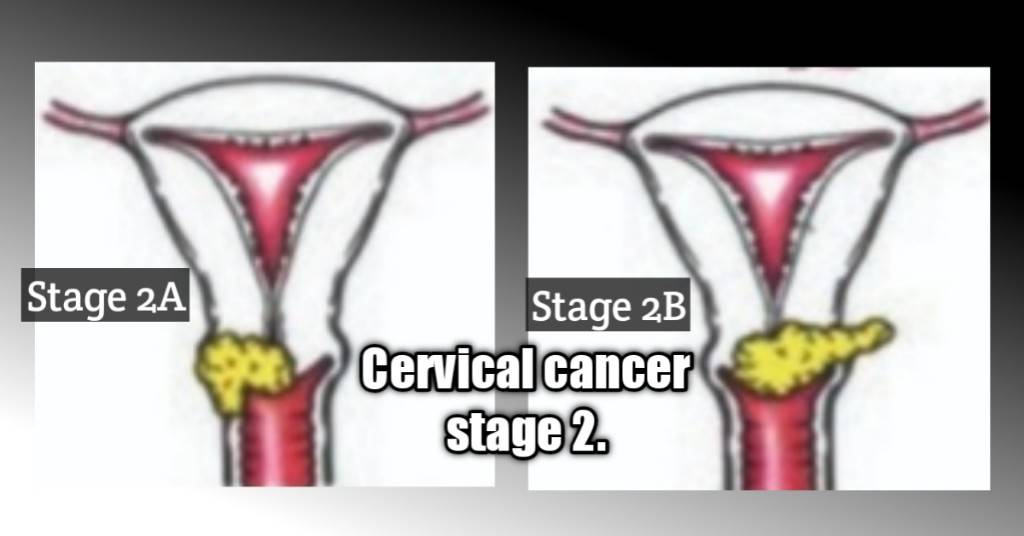
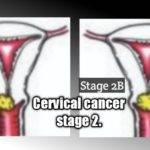
Cervical cancer stage 2 falls in the class of what is known as early-stage cervical cancer(stage 2A) or locally advanced cervical cancers(stage 2B). It’s the stage where cancer has spread from the cervix to the upper parts of the vagina or begun to spread to nearby tissues adjacent to the cervix.
It is usually discovered from abnormal pelvic examinations, pap smears, or certain symptoms known to characterize the presence of cervical cancer.
In this article, we’ll take a look at the divisions of stage 2 cervical cancer, the risk factors, symptoms, treatment, prognosis, and life expectancy.
The risk factors.
1. Untreated stage 1 or ineffective treatment, given at stage 1.
2. Discontinuation of screenings after a previous diagnosis and treatment of cancer. Someone who had been treated for stage 1 cervical cancer could have a relapse which if not discovered timely enough may progress to stage 2. This is why continuous screening is important.
3. Missed Vaccination or uncompleted vaccination. Majority of people get infected with the human papillomavirus at a point in their lifetime as mentioned in a previous article you may also be interested in. Vaccinations prepare your body’s defenses to fight off the infection when it occurs and completing your doses as recommended is what gives you adequate protection.
4. Smoking. It increases your chances of coming down with cervical cancer following an infection. This is due to its negative effects on your immunity, and its interference with healing and recovery.
5. Unprotected sex. The majority of HPV transmissions are via sex. Unprotected sex leaves you exposed to the virus.
6. Multiple sexual partners. Studies have shown the more lifetime sexual partners you have, the higher your chances of contracting the virus.
7. Existing sexually transmitted infection. People with sexually transmitted infections are known to be at higher risk.
8. Use of oral contraceptives. This increases your risk if used for a long time.
9. An HPV infection. HPV infections aren’t synonymous with cervical cancer as the body is usually able to fight off the virus within a year or two. However, in some cases, the infection could persist thereby paving the way for cancer.
10. Family history. For some reason, people with a family history of cervical cancer are at higher risk of coming down with the disease as has been acknowledged by the American Cancer Society (ACS).
11. Exposure to Diethylstilbestrol (DES). This is a synthetic type of the estrogen hormone given to pregnant women from 1940 to 1971 to prevent miscarriages but was stopped after it was linked to higher risks of developing cancerous tumors according to the National Cancer Institute (NCI).
Other factors include:
12. Early first-time sex. This influences the recommended age for vaccination as discussed in another article you may want to read. Vaccines are best given before exposure to the virus and the preteen ages of 11 to 12 years are targeted.
13. Early first pregnancy.
Stage 2 cervical cancer divisions.
Staging is very important in classifying cervical cancers in line with the size, the extent of metastasis, and the decision on the best treatment measures. In line with the International Federation of Gynecology and Obstetrics, stage 2 cancer describes the early point at which cervical cancer begins to spread beyond the cervix into adjacent tissues.(source)
It is divided into stages 2A and 2B.
Stage 2A.
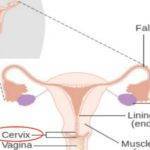
At this point, cervical cancer is seen to have spread from the cervix to the upper parts of the vagina as shown in the diagram above. This is classified as part of the early stages of cervical cancer along with stage 1 and has a comparatively better prognosis than subsequent stages.
It is further divided into two types. This division is based solely on the size of the tumor according to Cancer Research, UK (CRUK).
Tumors found to be up to 4cm in size but not more than that fall under stage 2A1 whereas those that are more than 4cm are tagged stage 2A2 cervical cancers.
Stage 2B.
At this stage, the cancer is found to have spread from the cervix to the tissues adjacent to the cervix or uterus as shown in the diagram below as acknowledged by the National Cancer Institute (NCI) and Cancer Research, UK (CRUK).
Stage 2b cervical cancer doesn’t fall in the class of early-stage cervical cancers. Rather, it is the first stage of a group called locally advanced cervical cancers according to the Canadian Cancer Society (CCS). At this point, everything begins to get more complicated.
The prognosis starts decreasing as cancer progresses and the survival rate starts falling.

Symptoms of stage 2 cervical cancer.
Whereas stage 2A cervical cancer may exist without symptoms in some cases, being early-stage cancer, it could still be discovered during regular screening. However, the locally advanced stages of which 2B is part, and the advanced stages are known to have the following symptoms.
- Abnormal vaginal bleeding may occur in post-menopausal women and between menses in premenopausal women.
- Pelvic pain and pain during intercourse.
- Foul-smelling vaginal discharge that may be watery, bloody, pink, or brown.
- Bleeding after coitus.
- Longer menses in premenopausal women.

Treatment for stage 2 cervical cancer.
Treatment is decided based on a couple of factors such as:
- Stage of cancer.
- Grade of cancer. (How many cancerous cells look like normal cells)
- Your medical history or existing medical conditions
- Your personal preferences or expectations like if you still want to have children after treatment.
- Type of cancer or type of cells from which they started.
Possible medical options in treating cervical cancers include:
- Surgery.
- Radiotherapy.
- Chemotherapy.
- Targeted drugs.
- Immunotherapy.
These treatment measures are often done in combination and chemoradiation is usually the preferred treatment choice for stage 2 cervical cancer. However, there may be slight variations between the treatment choices for stage 2A and 2B cancers.
During chemoradiation, external beam radiation therapy(EBRT) is given once daily, 5 times weekly for about 5 weeks. During the treatment, chemotherapy is given once weekly or after every 2 to 3 weeks.
Your treatment course is then rounded off with internal beam radiation, called intracavitary brachytherapy which is a type of brachytherapy for stage 2 cervical cancer treatment recognized by the Cancer Research, UK (CRUK), and the Canadian Cancer Society (CCS).
For once-weekly chemotherapy, Cisplatin may be the drug of choice for you, and for once every 3 weeks of chemo, cisplatin plus 5-fluorouracil may be administered.
3-dimensional conformal radiation therapy has been described which delivers targeted radiation specifically to the tumors in a way that spares surrounding tissues and organs from the radiation according to the American Cancer Society (ACS).1
If you were diagnosed with stage 2A cervical cancer, surgery may be considered in addition to either radiation therapy or chemoradiation. Your choice of surgery will depend on your desire to have children or not, post-treatment. You’ll either have to settle for a radical trachelectomy or a hysterectomy.
Trachelectomy: This is a fertility-preserving procedure and involves the surgical excision of the cervix along with the upper parts of the vagina and is ideal for younger women who desire to have children. An ideal mode of delivery after this procedure is a cesarean section. (source)
Hysterectomy: This is for those with stage 2A cancer who wouldn’t want to have babies after the treatment as it involves the removal of the uterus or womb.
keep in touch. Subscribe to our newsletter.
Prognosis
Several factors are considered in determining your prognosis. These include the type of cancer, stage at diagnosis, age, tumor size, health, and HIV status as stated by the National Cancer Institute (NCI), and the Canadian Cancer Society (CCS).
Generally, the early stages of any cancer signify a better prognosis than the later stages. Also, the younger you are, the better. The size of the tumor has a lot to do with the stage and smaller sizes which may mean earlier stages, give a better prognosis.
Having an underlying disease like HIV will hurt your prognosis. In summary, where all these considerations are equal, cervical cancer stage 2 has a better prognosis(only second to stage 1) than the more advanced ones.
Life expectancy.
This differs among individuals on the same factors used to determine the prognosis. The Cancer Research, UK (CRUK) stated that about 70 out of every 100 women found to have stage 2 cervical cancer are known to live for the next 5 years from the date of diagnosis.
This doesn’t mean after 5 years everyone dies. The majority of treatments at this stage are quite successful and the patients live the rest of their lives cancer-free and in relatively good health. Some people do experience a recurrence though.
You may also want to find out exclusively about the locally advanced stage 3, and the advanced stage 4 cancers.
Reference.
- Minn, A. Y., Hsu, A., La, T., Kunz, P., Fisher, G. A., Ford, J. M., Norton, J. A., Visser, B., Goodman, K. A., Koong, A. C., & Chang, D. T. (2010). Comparison of intensity-modulated radiotherapy and 3-dimensional conformal radiotherapy as adjuvant therapy for gastric cancer. Cancer, 116(16), 3943-3952. https://doi.org/10.1002/cncr.25246 ↩︎


























































































































I have been browsing online more than 3 hours today, yet I never found any interesting article like yours. It is pretty note worthy. In my opinion, if all web owners and bloggers made good content as you did, the internet will be a lot more useful than ever before.
Thank you for all of the effort on this web site. Enjoy the remaining part of the new year. You are always doing a fantastic job.